Pulmonary embolism (PE) is a pathological entity that occurs when a venous emboli travels through the venous circulatory system to the right heart cavities, subsequently being caught within the pulmonary arteries. It is one of the most frequent pathologies that radiologists find in a clinical setting, especially in an emergency environment. Accurate diagnosis is pivotal, as it might be a life-threatening condition that may warrant active intervention, according to severity.
The signs and symptoms of PE are non-specific and hence this pathology is characterised by a broad spectrum of clinical presentations. PE may be totally asymptomatic and discovered incidentally during diagnostic workup for another disease or show common, although nonspecific signs and symptoms like dyspnoea, chest pain, haemoptysis and in more severe cases syncope, haemodynamic instability and cardiac arrest. In addition to symptoms, knowledge of the predisposing factors for venous thromboembolism is important in determining the clinical probability of the disease. The combination of signs, symptoms and predisposing factors allows for the classification of patients with suspected PE into three categories of pre-test probability (low, intermediate and high), which correspond to an increasing actual prevalence of confirmed PE. There are various scores, with the most established ones being the Geneva and Wells scores, to categorize this pre-test probability. Simplified versions of these scores have been created to be used routinely in clinical practice. To avoid overuse of diagnostic tests for pulmonary embolism, D-dimer levels should be requested for patients with low to intermediate probability for PE, as it has a high negative predictive value and a normal D-dimer level renders acute PE unlikely. On the other hand, the positive predictive value of elevated D-dimer levels is low and can be elevated in various situations like cancer, infection and pregnancy. In patients with high probability for PE, imaging methods should be performed without the need for D-dimer level.
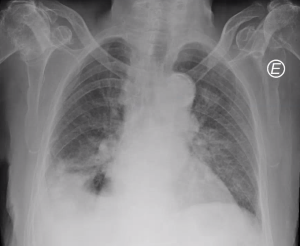
Chest radiography can be mostly performed to exclude alternative diagnosis. In some situations, some signs on chest radiography can be present that indicate PE, such as the Fleischner, Hampton or Westermark sign, although these are neither sensitive nor specific.
Other imaging methods, such as magnetic resonance imaging (MRI) and nuclear imaging play an important role when CTPA is contra-indicated, such as during pregnancy or in patients allergic to iodinated IV contrast.
In any case, CTPA remains the gold-standard. It is fast, readily available and has excellent accuracy. CTPA is conventionally performed by acquiring images of the whole thorax after intravenous contrast administration in the pulmonary arterial phase, with the objective of optimal opacification of pulmonary arteries up to the subsegmental branches. Exposure to ionising radiation and the need for administration of iodinated IV contrast, with its potential for nephrotoxicity, are its main disadvantages.