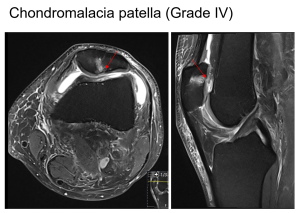
A) OSTEOCHONDRAL LESIONS
The mature osteochondral unit includes smooth joint cartilage, the bone plate beneath it, and the spongy bone underneath [1]. Healthy articular cartilage contains a small number of chondrocytes (1%-5% by volume), and the majority of the tissue is composed of an extracellular matrix that contains water (65%-85%), collagen (10%-20% by wet weight), and proteoglycans (5%-10% by wet weight) [1]. Articular cartilage has four zones: the superficial (tangential) zone, middle (transitional) zone, deep (radial) zone, and the calcified zone [1].
Osteochondral lesions of the knee can arise from various causes, and differentiating between them can be challenging, especially when imaging findings overlap. Patient demographics, clinical presentation, and trauma history are key to distinguishing these conditions. Osteochondral defects can result from acute injury or chronic issues [2].
Key MRI findings include bone marrow edema, fractures, subchondral changes, and deformities in the subchondral bone plate [2].
Common conditions include acute traumatic osteochondral injuries, subchondral insufficiency fractures (such as spontaneous osteonecrosis of the knee), avascular necrosis, osteochondritis dissecans, and localized osteochondral changes seen in osteoarthritis [2].
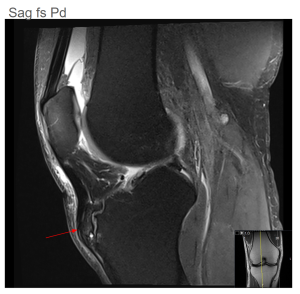
Osteochondritis dissecans refers to an injury caused by repeated small trauma to the developing subchondral bone, which disrupts endochondral ossification and increases the risk of instability in the osteochondral unit. If the condition does not heal, it can progress from a signal similar to subchondral edema to an actual osteochondral defect (Figure 2) [3].

Osteochondral lesions in the knee can be detected with MRI by the presence of a high T2 signal for edema and a low T1 signal for necrosis, emphasizing important changes in the subchondral area [2].
The choice of MRI sequence affects how cartilage damage is graded by influencing the clarity of the articular surface, bone, and cartilage signal. T1-weighted sequences have poor contrast, making superficial lesions hard to detect without an arthrogram. T2-weighted sequences provide better contrast but may struggle to show the bone plate and lesion depth due to lower cartilage signal intensity. Proton-density and intermediate-weighted sequences offer the best signal quality and resolution, helping to distinguish cartilage from joint fluid and bone [1].
To assess the collagen structure and proteoglycan levels in knee cartilage, techniques such as T2 mapping, delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), T1ρ imaging, sodium imaging, and diffusion-weighted imaging are used. These methods can be combined and applied at different magnetic field strengths in both clinical and research environments to better characterize changes in cartilage composition [4].
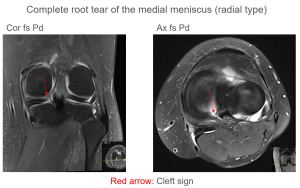
B) MENISCAL TEARS
The lateral and medial menisci are C-shaped cartilage structures that cover 70% of the tibial plateau, aiding in shock absorption and weight distribution. The inner two-thirds have no blood supply, while the outer third is well-vascularized. The menisci also contain nerve endings for joint awareness. The medial meniscus is less mobile due to its firmer attachments, while the lateral meniscus is more flexible and connects to the femur via ligaments [5].
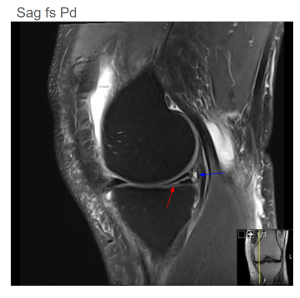
Meniscal tears are classified by shape and location on MRI. Horizontal tears are parallel to the tibial plateau and are common in older adults with degeneration (Figure 3). Longitudinal tears run perpendicular to the plateau, while radial tears are perpendicular to both the plateau and meniscus axis (Figure 4 and Figure 5). Complex tears combine different types, and displaced tears involve detachment or flipping. Bucket-handle tears are displaced longitudinal tears (Figure 6 and Figure 7), and parrot-beak tears are partially detached radial tears. Flap tears are partially detached horizontal fragments (Figure 8). Red-red tears in the outer vascular zone heal the best, while red-white and white-white tears in the avascular zone are less likely to heal [5,6].
MRI is the best method for diagnosing meniscal tears, with high sensitivity and specificity (93%/88% for medial meniscal tears and 79%/96% for lateral meniscal tears).
On T2-weighted images, tears appear as high signal intensity areas within the low signal intensity of the normal meniscus, indicating fluid accumulation.
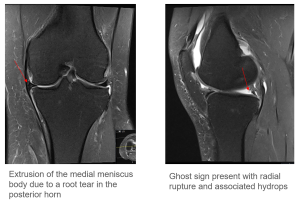

For patients with persistent pain, swelling, and mechanical issues despite conservative treatment, surgery may be required. Meniscal repair is preferred over meniscectomy to prevent the development of osteoarthritis, as removing the meniscus decreases cushioning and increases cartilage stress. Repair success is higher with tears located in the red zone, smaller tears, and acute or vertical tears. Post-surgery rehabilitation includes limiting knee flexion and weight-bearing in the first 6 weeks, and meniscal allograft transplantation may be an option for patients under 50 with a meniscus-deficient knee [5,7].
C) LIGAMENT INJURY
The four primary ligaments that stabilize the knee are the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) [8].
Ligaments typically appear as low-signal intensity structures on T1-, T2-, and PD-weighted imaging sequences [9].
The cruciate ligaments consist of two bundles, visible in all imaging planes, with the anterior cruciate ligament (ACL) showing more striation than the posterior cruciate ligament (PCL). This appearance should not be mistaken for a partial tear of the ACL. Ligament abnormalities are characterized by increased signal intensity, abnormal thickening or thinning, or fiber disruption. Bony avulsions at the origin or insertion points of the cruciate and collateral ligaments should also be documented [10].
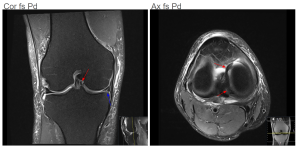
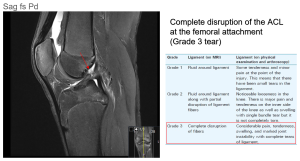
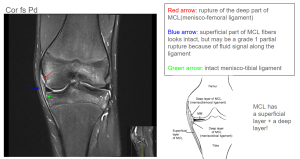
Ligament injuries should be classified as either full-thickness or partial-thickness tears, taking into account the limitations of MRI in identifying partial tears. It is also important to assess for indirect signs of ligament instability or absence, along with evaluating joint alignment, to improve diagnostic accuracy (Figure 9 and Figure 10) [3].
D) BONE LESIONS
MRI sequences for bone lesions include T1-weighted (for anatomical detail), T2-weighted and STIR (for edema detection), and fat-suppressed sequences (to highlight marrow abnormalities), which are used to assess fractures, tumors, or inflammation.
Unexpected bone lesions often pose a diagnostic challenge. Retrospective studies show that the occurrence of unexpected musculoskeletal findings ranges from 2% to 10%. When a bone lesion is first identified on MRI, conventional X-rays should be obtained for comparison. The radiographs help assess important characteristics of the lesion, such as its edges, periosteal response, and matrix [11].
The margin of a bone lesion plays an important role in determining its aggressiveness, with a sclerotic margin indicating slow growth and a lower chance of malignancy (under 6%). On the other hand, geographic osteolytic lesions with poorly defined borders have about a 50% likelihood of being malignant, while permeative lesions carry a greater than 80% chance. The type of matrix—cartilage, bone, or fibrous tissue—can help distinguish between different bone tumors, although identifying the matrix on MRI can be challenging. Primary bone sarcomas are uncommon, representing less than 0.2% of bone cancers, whereas metastatic cancers, such as those from the breast, lung, and prostate, are more commonly seen. It's important to take a comprehensive approach when evaluating a bone lesion, considering a wide range of potential diagnoses, including tumors, infections, trauma, and other conditions, to ensure the correct diagnosis is made [12,13].
E) OTHER STRUCTURES
Hoffa's fat pad cushions and stabilizes the anterior knee joint. Inflammation or fibrosis can cause discomfort. Anterior knee pain may result from patellar malalignment, linked to ACL injuries. In this setting, MRI signs such as patellar lateralization or abnormal sulcus depth suggest a risk of subluxation. Surrounding tissues may show neural cysts, nerve damage, or muscle denervation. A comprehensive assessment is crucial to detect tendon injuries or fractures in acute trauma cases [3,14].
