CT offers several advantages for detecting PNS, including superior spatial resolution, reduced sensitivity to motion, excellent fat–soft tissue contrast, and clear depiction of blood vessels that commonly run alongside nerves. In the upper abdomen, nerves are generally small and sparse to be directly visualized, making arterial branches reliable surrogates for neural pathways. Because recognition of PNS in this region relies on detecting subtle changes in the fat planes surrounding these vessels, CT outperforms MRI for evaluation of upper abdominal PNS.
In contrast, MRI is ideal for imaging PNS along the lumbosacral plexus in the pelvis, as the nerve roots and associated branches are larger and more discrete, allowing direct visualization.
Radiologically, PNS can manifest either as abnormal soft-tissue attenuation extending along nerve routes(perivascular soft tissue) or as direct involvement of the tumor with the adjacent nerve roots or branches.
ABDOMEN
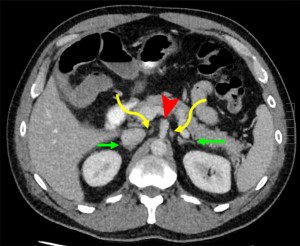
The celiac plexus is a key anatomic landmark in detecting PNS. As the largest autonomic plexus, it forms a dense network of interconnecting nerve fibers in the upper abdomen.
The celiac plexus is located in the retroperitoneum and consists of the right and left celiac ganglia along with the superior mesenteric ganglion. Each celiac ganglion lies on either side of the celiac trunk, medial to the adrenal glands, following their corresponding arterial vasculature. On CT, the ganglia exhibit a characteristic “discoid” or multilobulated appearance, best appreciated on axial images .
The most common abdominal malignancies to reveal PNS include cancers of the pancreas, bile ducts (extra- and intrahepatic), gallbladder, and stomach.
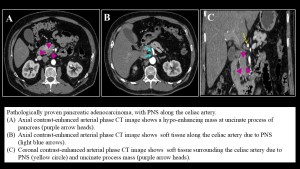
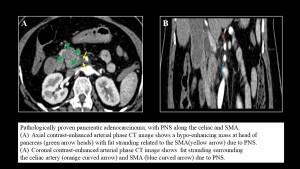
Pancreatic cancer
The tendency of pancreatic cancer to spread along nerves is likely attributable to the dense network of neural plexuses surrounding the pancreas. In pancreatic ductal adenocarcinoma, the most frequent sites of perineural spread are the celiac plexus and the plexus pancreaticus capitalis . Except for the celiac ganglia, the neural plexuses are not directly visualized at imaging, with the mesenteric arteries they follow serving as surrogate landmarks for detection, where PNS manifest as wispy increased attenuation or confluent perivascular soft tissue.

Cholangiocarcinoma
Cholangiocarcinoma, whether extrahepatic or intrahepatic, is an aggressive malignancy with poor prognosis. Recurrence is often driven by nodal metastases and extensive perineural spread.
- In extrahepatic tumors, PNS typically occurs through the posterior hepatic plexus, a large tributary of the celiac plexus along the common hepatic artery as well as the posterior inferior pancreaticoduodenal artery and the superior mesenteric artery.
 Fig 5: Illustration shows the posterior hepatic plexus (yellow arrow), a large tributary of the celiac plexus along the common hepatic artery (arrowhead). This supplies branches to the extrahepatic bile duct and gallbladder including the superior, middle, and inferior common bile duct (green arrow), portal vein (purple arrow), and nerves (yellow arrow).
Fig 5: Illustration shows the posterior hepatic plexus (yellow arrow), a large tributary of the celiac plexus along the common hepatic artery (arrowhead). This supplies branches to the extrahepatic bile duct and gallbladder including the superior, middle, and inferior common bile duct (green arrow), portal vein (purple arrow), and nerves (yellow arrow).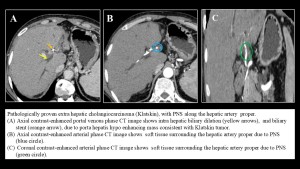
- In intrahepatic tumors, right-lobe lesions spread along the common hepatic artery, while left-lobe lesions follow the left gastric artery. Both pathways ultimately lead to involvement of celiac ganglia.
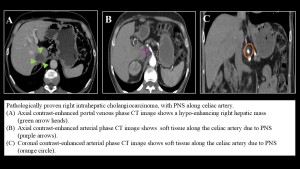

Gall bladder carcinoma may also demonstrate perineural spread, likely around the common hepatic artery, celiac artery, and superior mesenteric artery .
Gastric cancer may exhibit PNS through perivascular nerve plexuses associated with the left gastric artery, common hepatic artery, and celiac artery.
PELVIS
Pelvic organs have complex innervation, and malignancies can infiltrate pelvic nerves, causing pain, sensory and motor deficits, as well as autonomic dysfunction. A key neural structure is the lumbosacral plexus. The plexus gives rise to several branches, but only the sciatic, pudendal, femoral, and obturator nerves are reliably visualized on MRI. For autonomic innervation, the superior and inferior hypogastric plexuses are essential.
The inferior hypogastric plexus is a key structure to examine in patients with common pelvic malignancies because it innervates major pelvic organs through the vesicoureteric plexus, the rectal plexus, the uterovaginal plexus in female patients, and the prostatic plexus in male patients.
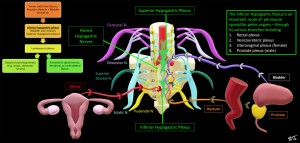
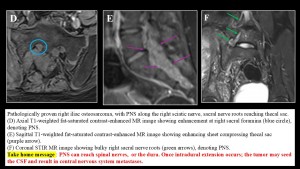
Pelvic tumors can invade the inferior hypogastric plexus, which connects to the lumbosacral plexus, allowing tumor spread distally to major nerves (eg; sciatic) or proximally to spinal nerves, the contralateral plexus, or the dura. Intradural extension may enable tumor cells to enter the cerebrospinal fluid, potentially leading to central nervous system metastases.
The most common primary tumors causing lumbosacral plexopathy, include colo-rectal cancer, sarcomas, breast tumors, lymphomas, cervical tumors, melanomas, and tumors of bladder, prostate, and uterus.
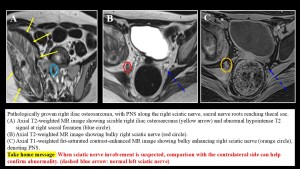
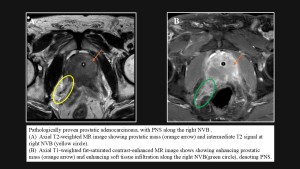
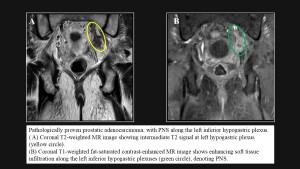
MRI features of PNS :
- Nerve enlargement on T1-weighted images.
- Abnormal signal on T2-weighted images.
- Perineural enhancement on contrast-enhanced sequences.
Prostatic cancer
In prostatic cancer, perineural spread commonly involves the neurovascular bundle (NVB), which can be readily visualized on MRI and is considered a component of extraprostatic extension. Accurate detection of NVB involvement is critical for management, influencing decisions regarding surgery and the need for adjuvant therapies. On MRI, the NVB is located along the dorsolateral prostate and anterolateral rectum. Normally, it appears as low-signal-intensity foci within a triangular or round area of hyperintense fat at the prostate base and mid-gland on T1- and T2-weighted images. Involvement is suggested by asymmetrically enlarged nerves compared with the contralateral side, indicating tumor infiltration along the nerve sheaths.
Rectal cancer
In rectal cancer, perineural spread carries a poorer prognosis .Tumor may track along the lumbosacral plexus, sciatic, obturator, and spinal nerves, frequently starting with the inferior hypogastric plexus. On imaging, PNS appears as nodular thickening and enhancement of the perirectal fascia extending toward the lumbosacral plexus. This plexopathy may result from direct tumor infiltration or metastatic deposits.
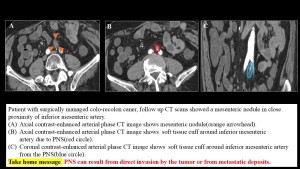
A similar pattern of PNS can occur in other pelvic malignancies, including cervical, uterine, ovarian, bladder cancers, as well as pelvic sarcoma . The superior hypogastric plexus, may serve as an additional conduit for tumor spread.