Virtual Surgical Planning in Maxillofacial Surgery
Virtual surgical planning has transformed maxillofacial surgery, enhancing the precision of complex procedures [1][2]. Using preoperative Computed Tomography (CT) and/or Magnetic Resonance Imaging (MRI), this planning incorporates advanced techniques such as 3D visualization, virtual reality, 3D-printed models, and customized 3D-printed surgical guides.
Despite these advancements, achieving exact alignment between surgical execution and the preoperative plan remains challenging. Usually, radiological evaluations of surgical outcomes—especially in orthognathic and distraction osteogenesis surgeries—are performed postoperatively, often weeks after the procedure, using postoperative CT scans. This delayed feedback can leave deviations or issues unaddressed during surgery.
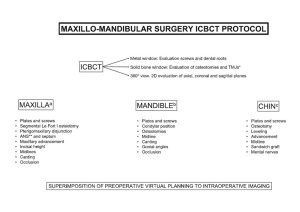
Incorporating intraoperative cone beam CT (CBCT) imaging into the workflow allows for real-time visualization of radiological landmarks and anatomical structures [3]. This enables the immediate detection and correction of discrepancies between the surgical plan and intraoperative outcomes [4], improving accuracy and reducing the need for future revisions.
Study Overview
The study was conducted in accordance with the Code of Ethics of the World Medical Association (Declaration oh Helsinki) and approved by Ethics Comitee at Sant Joan de Déu Barcelona Children's Hospital.
A total of 150 complex paediatric maxillofacial procedures—including orthognathic surgery, maxillary and mandibular distractions, and Le Fort III distractions—were performed in an operating room equipped with an intraoperative CBCT (Fig. 1). A low-dose CBCT protocol (0.56 mSv per acquisition) was utilised to minimize radiation exposure.

Patients were positioned supine, intubated under general anesthesia, with their heads oriented towards the C-arm CBCT. To ensure optimal imaging, an X-ray transparent head support and long tubes were employed. For orthognathic procedures, elastic intermaxillary fixation was applied to minimize wire artifacts. Prior to surgery, the C-arm CBCT was calibrated by a radiology technician.
Workflow
Following surgical corrections, intraoperative CBCT scans were acquired and images were analysed by surgeons intraoperatively (Fig. 2). The images were used to determine whether immediate refinements were required, with repeat CBCT scans performed as necessary.

A standardized checklist guided the evaluation for orthognathic and distraction osteogenesis surgeries, ensuring thorough and consistent assessments (Fig. 3).