All the women with a diagnosis of endometriosis (105 patients) were retrospectively selected between June 2018 and May 2024, using pelvic magnetic resonance imaging (MRI). Currently, MRI is considered the best imaging technique for mapping endometriosis, since it provides a more reliable map of deep infiltrating endometriosis than physical examination and transvaginal ultrasound (TVUS) [9]. We also retrospectively selected 120 patients, extracted from our database, who had the finding of retroverted uterus on MRI report, examined in a time period from June 2018 to May 2024.
Inclusion criteria: women with a retroverted uterus in young or fertile age, the type of examination performed had to be an MRI aimed at studying the pelvis or including it, sometimes even indicating the finding only as incidental. Patients with advanced age as menopausal or whose examination was not suitable for technical reasons were successively excluded. Based on these criteria 23 patients were discarded, leaving 97 patients for image analysis, which were divided into three groups
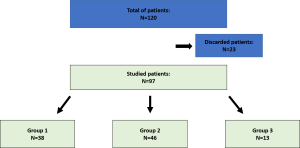
- Women with a history or strong clinical suspicion of endometriosis or with diagnosis (38 patients);
- Women without diagnosis of endometriosis but with MR findings suggestive of endometriosis (46 patients);
- Women with a retroverted uterus likely due to other causes (cesarean section, post-surgical adhesions, etc., 13 patients).
MR imaging is performed with a closed-configuration superconducting 1.5-T system (Signa HDxT; GE Healthcare, Milwaukee, WI, USA), by using an eight-channel high-resolution surface phased-array torso coil with array spatial sensitivity technique (ASSET) parallel acquisition.
MR imaging protocol we use to study patients with pelvic endometriosis is:
- Standard three-plane scout image;
- axial T2-weighted single-shot fast spin echo (SSFSE);
- sagittal T2-weighted fast recovery fast spin echo (FRFSE);
- oblique/coronal/axial T2-weighted fast recovery fast spin echo (FRFSE);
- axial T2*;
- axial DWI spin echo echoplanar imaging (SE EPI);
- Sagittal, oblique coronal/axial T1 weighted 3D gradient echo LAVA fat-suppressed sequence.
The MR examinations were evaluated by two radiologists in consensus. In addition to the identification of a retroflexed uterus, other associated findings, which confirmed the diagnosis of endometriosis or which were suggestive, were noted. These included the presence of endometriotic ovarian implants, retro-cervical implants or adhesions, adhesions in the posterior vaginal fornix or posterior wall/ischial body, thickening of the uterosacral ligament (USL) and round ligament (LR), involvement of the bladder, sigmoid colon, ileal loops, diaphragm, rectum, fallopian tubes, signs of kissing ovaries, and typical endometriotic shading. Other findings include: leiomyomas (about 10), ovarian or endometrial neoplastic formations, outcomes of previous pregnancies or cesarean deliveries, or collateral findings such as fistulas or pelvic prolapses.