
Neuroendovascular therapy (NET) has become a standard minimally invasive approach for the treatment of intracranial aneurysms. Despite its clinical advantages, NET requires extensive use of fluoroscopy and digital subtraction angiography (DSA), resulting in relatively high radiation exposure compared with other interventional procedures. Radiation-induced skin injury such as epilation is therefore a major safety issue, especially considering that the peak skin dose (PSD) is strongly influenced by cumulative fluoroscopy and repeated DSA exposures(1, 2) (figure1 and figure2).
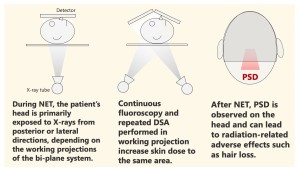
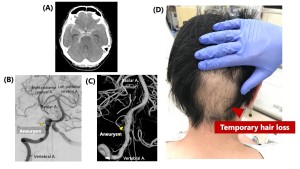
In clinical practice, identifying the precise PSD location is crucial for preventing deterministic effects including epilation. However, the PSD location in NET is difficult to predict because the frontal and lateral X-ray tubes dynamically alter their angulation in both craniocaudal and oblique directions throughout the workflow of angiography. Although several case-based reports have described PSD distribution patterns (3-5), no prior study has systematically investigated which patient- or procedure-related factors determine PSD location.
This study aimed to:
- Identify the most frequent PSD location during NET for unruptured aneurysms using a direct dosimetry technique.
- Determine clinical and procedural predictors associated with PSD distribution.
- Provide insights that may support radiation risk prediction and improve radiation protection strategies in NET.