Findings and procedure details
Common indications for shoulder arthroplasty include osteoarthritis (the leading cause), inflammatory arthritis, complex proximal humerus fractures, irreparable rotator cuff tears, rotator cuff arthropathy and avascular necrosis (AVN) of the humeral head.
The choice of arthroplasty type is determined by the underlying pathology. Partial joint replacement is typically favoured in younger patients with isolated humeral head abnormalities, while conditions involving both sides of the joint necessitate total shoulder arthroplasty. Anatomic total shoulder arthroplasty requires intact rotator cuff. When compromised, RTSA is indicated and involves reversing the natural ball-and-socket anatomy.
We will now describe different types of shoulder arthroplasty, their specific complications, followed by complications which are generalized to all types.
Partial joint replacement
Partial joint replacement is typically designed to treat younger patients with humeral head abnormalities (e.g., fracture or AVN) and include humeral head resurfacing (partial or complete) or hemiarthroplasty. In humeral head resurfacing, which preserves bone stock and maintains more of the native bone structure, the humeral head is reamed, and a metal-alloy cap is placed. Hemiarthroplasty, on the other hand, addresses more advanced pathological conditions affecting the humeral side of the joint, such as three- or four-part proximal humerus fractures or advanced AVN. This procedure involves the insertion of a stemmed metal humeral component without incorporating a glenoid component.
Radiographically, a properly positioned humeral stem should be centered within the humeral shaft, and the humeral head should be aligned and centered within the glenoid.
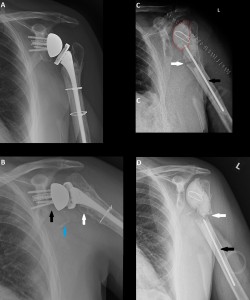
Fig 1: Case A. Anteroposterior shoulder radiograph showing complete humeral head resurfacing arthroplasty with the cap flush against the bone; no lucency around the peg.
Case B. Anteroposterior shoulder radiograph showing normal shoulder hemiarthroplasty with the stem centered within the humeral shaft and the head centered within the glenoid.
©”Lin D et al. (2016) Shoulder arthroplasty, from indications to complications: What the radiologist needs to know. Radiographics 36:192-208”
* Glenoid side pathology
The primary complication associated with partial joint replacement is the development of pathological conditions on the native glenoid side of the joint, most commonly osteoarthritis. This often necessitates revision to total shoulder arthroplasty. Typical findings of osteoarthritis should be assessed, including progressive joint space narrowing and posterior glenoid wear.
Fig 2: Case A. Anteroposterior radiograph of a 44-year-old man obtained 4 years after complete resurfacing arthroplasty shows glenoid osteoarthritis with joint space narrowing (white arrow) and subchondral cyst formation (black arrow).
Case B. Axillary radiograph of the same patient shows glenoid osteoarthritis with a typical pattern of posterior glenoid wear (arrow)
©”Lin D et al. (2016) Shoulder arthroplasty, from indications to complications: What the radiologist needs to know. Radiographics 36:192-208”
Anatomic total shoulder arthroplasty (TSA)
TSA preserves the natural ball-and-socket morphology of the glenohumeral joint and is used to treat pathologies involving both sides of the joint, such as osteoarthritis and inflammatory arthritis. Revision of a failed partial arthroplasty is another common indication. This procedure requires an intact rotator cuff, as TSA relies on the function of native soft tissues, as well as adequate glenoid bone stock to ensure proper glenoid component placement.
TSA involves the use of a stemmed metal humeral component and a glenoid component. Modern glenoid components are predominantly made of radiolucent polyethylene, which has replaced older metallic designs due to their higher failure rates and reduced durability. A small radiopaque marker is embedded within the central peg to allow assessment of proper positioning on following imaging.
Fig 3: Illustration of total shoulder arthroplasty components. Stemmed metallic humeral component (thick arrow) and the radiolucent polyethylene glenoid component.
©”Lin D et al. (2016) Shoulder arthroplasty, from indications to complications: What the radiologist needs to know. Radiographics 36:192-208”
Fig 4: Anteroposterior (A) and scapular Y (B) radiographs of normal findings in a patient with total shoulder arthroplasty. The humeral stem (thick arrows) is centered within the humeral shaft, and the humeral prosthetic head is centered within the glenoid component (thin arrow).
©”Combes D et al. (2019) Imaging of shoulder arthroplasties and their complications: a pictorial review. Insights into Imaging 10”
* Glenoid Component loosening
Most common TSA complication (37%), and roughly 4.5 times more frequent than humeral component loosening. An incomplete periprosthetic lucent line less than 1.5 mm is a common and nonspecific finding. If the lucency is exceeding 1.5 mm or progressive on serial radiographs, loosening is indicated. Additional findings indicative of loosening include component failure (dislocation, migration, tilt and subsidence). Eccentric loading is associated with glenoid component failure and may result from retroversion installation of the component or rotator cuff deficiency. A subscapularis tear is the most common soft tissue complication and is related to its temporary detachment, required during surgery, which is necessary to allow access to the joint.
Fig 5: Anteroposterior (A) and axillary view (B) radiographs of a 70-year-old woman with pain and dislocations after anatomic TSA. There is a radiopaque glenoid component marker (white arrow) within the anterioinferior joint space, in addition to an empty and ill-defined glenoid fossa (*). The findings are compatible with glenoid component loosening resulting in its dislocation.
©”Lin D et al. (2016) Shoulder arthroplasty, from indications to complications: What the radiologist needs to know. Radiographics 36:192-208”
Fig 6: Anteroposterior (A) and axillary view (B) radiographs of a 78-year-old man, two years after a left anatomic TSA. Humeral stemless component is unremarkable and centered within the glenoid component. The radiopaque marker within the central peg is properly located in the glenoid. There is a thin, less than 1.5 mm lucency around the glenoid component, involving the mid- inferior portion (black arrow), with sparing of the superior aspect. Almost three years later, anteroposterior (C) and axillary view (D) radiographs show stability of the findings. This thin, non-progressive lucency is non-specific, and not suggestive of loosening.
Reverse total shoulder arthroplasty (RTSA)
As the name suggests, RTSA reverses the ball and socket of the shoulder joint and is designed for patients with rotator cuff deficiencies. These patients are not candidates for anatomic TSA, because without the stabilizing effect of the rotator cuff, rapid loosening of the glenoid component can occur. In RTSA, the centre of rotation is shifted distally and medially, improving leverage and control of deltoid muscle, that replaces deficient rotator cuff as shoulder abductor.
The Glenoid component is modular, consisting of a base, called metaglene, which is anchored into the native glenoid with screws. A round glenosphere is secured to the metaglene. The humeral component consists of a metal stem, either cemented or non-cemented. Customizable cup-shaped polyethylene is attached to the stem, articulating with the glenosphere.
Fig 7: Photograph of a reverse shoulder arthroplasty before implantation in the operating room. (a) Complete prosthesis. The yellow part attached to the humeral stem is the polyethylene cup. (b) Metaglene. (c) Glenosphere.
©”Combes D et al. (2019) Imaging of shoulder arthroplasties and their complications: a pictorial review. Insights into Imaging 10”
Fig 8: Anteroposterior (A), scapular Y (B), and axillary (C) radiographs of normal findings in a patient with reverse shoulder arthroplasty. The humeral stem (thick arrows) is centered within the humeral shaft. The glenosphere (thin arrows) is placed flush with the native glenoid and the humeral component is centered on the glenosphere.
©”Combes D et al. (2019) Imaging of shoulder arthroplasties and their complications: a pictorial review. Insights into Imaging 2019”
* Dislocation (anterosuperior)
The most common early complication, occurring in 20% of patients, often arises without any trauma. Unlike native shoulder dislocation, which is mostly anteroinferior, in RTSA the dislocated humeral component usually lies anteriorly and superiorly to the glenoid component. This is attributed to the pull of the deltoid muscle, unopposed by deficient rotator cuff muscles.
Fig 9: Anteroposterior (A) and axillary (B) radiographs of a 56 year-old male after right reverse shoulder arthroplasty. The humeral component is abnormally located superiorly and anteriorly in relation to the glenosphere. This is compatible with dislocation.
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
* Scapular Notching
An exceedingly common complication (50%-96%), scapular notching is caused by repetitive contact between the polyethylene humeral cup and the inferior scapular border, likely related to the previously mentioned medialization of the joint's centre. Its clinical significance is debatable; while patients are often asymptomatic, some studies suggest correlation with decreased range of motion. Scapular notching severity can be graded by Sirvenaux classification. Lower grades typically require no treatment, but higher grades may result in glenosphere loosening and occasionally necessitate surgical revision.
Fig 10: Anteroposterior radiograph in an elderly male, seven years after right reverse shoulder arthroplasty. There is a small focal lucency at the inferior aspect of the scapula, involving the glenoid component pilar (black arrow), compatible with grade 1 scapular notching. The Sirvenaux classification grades scapular notching as follows: Grade 1 is limited to the pillar; Grade 2 involves the lower metaglene screw; Grade 3 extends over the entire inferior metaglene screw; and Grade 4 includes extension under metaglene baseplate. Grades 3 and 4 may necessitate revision surgery.
Additionally, there is focal lucency and remodeling at the medial aspect of the periprosthetic humerus (white arrow) and coarse ossification inferior-posterior to the joint (blue asterisk), the latter is consistent with heterotopic ossification.
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
* Acromial / scapular fracture
This complication occurs in 5-7% of patients and is considered a stress-fracture. As explained above, the deltoid muscle replaces the rotator cuff as shoulder abductor in RTSA, increasing stress on the acromion. These fractures are usually divided into 3 types: Type 1 involves the anterior acromion near or including the coracoacromial ligament footprint, Type 2 occurs in anterior acromion just posterior to the acromioclavicular joint and Type 3 fractures are located in the posterior acromion or scapular spine.
Fig 11: Anteroposterior (A) and axillary view (B) radiographs of a 79-year-old man, five months after a left RTSA show a mildly distracted type 2 acromial fracture (black arrow). The acromion was normal on prior radiographs, meaning it is indeed a fracture, rather than an Os-Acromiale.
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
General complications seen in all arthroplasty types
* Periprosthetic fracture
Accounts for 11% of all complications, occurs across all types, though more common after RTSA. Can be intraoperative or most commonly, postoperative. Fractures are often centred around the distal part of the humeral stem. Loosening and stress shielding (local bone demineralization) are a predisposing risk factor for periprosthetic fracture. Fig. 13 illustrates Worland et al. classification system for periprosthetic fractures.
Fig 12: Anteroposterior (A) and axillary view (B) radiographs of a 75-year-old man, five years after a left RTSA, demonstrate diffuse lucency around the humeral stem (black arrows), in the bone-cement interface, most pronounced near the tip. This lucency is larger than 1.5 mm and progressive, compared to older radiographs (not shown). Small associated cement fracture is noted (white arrow). A few months later, anteroposterior (C) and oblique (D) radiographs reveal a mildly comminuted and angulated periprosthetic fracture around the humeral stem tip (blue arrow).
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
Fig 13: (As detailed in the image)
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
* Loosening
Glenoid component loosening is the most common complication specific to TSA, as mentioned above. However, loosening, and in particular of the humeral component, is relevant for all arthroplasty types. It is rare, with an incidence of less than 1%, and is suspected when larger than 1.5 mm or progressive periprosthetic lucency is present. Other signs include component tilt or subsidence.
Fig 14: Anteroposterior (A) and axillary view (B) radiographs of an elderly man, seven years after a left RTSA show marked diffuse loosening around the humeral component (black arrows), accompanied by subsidence (white arrow). Nondisplaced subacute periprosthetic fracture is evident in the axillary radiograph, within the posterior cortex of the proximal humerus (blue arrow).
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
* Hardware failure
This wide term harbors hardware breakage (e.g. fixation screws), dissociation of polyethylene, glenosphere or humeral components etc.
Fig 15: Anteroposterior (A) and axillary (B) radiographs of an elderly male, eight years after a right RTSA, demonstrate a fracture in the posterior most fixation screw (black arrows). In addition, there is mild lucency in the inferior aspect of glenoid, involving the lower metaglene screw - suggestive of grade 2 scapular notching (white arrow).
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
* Infection
Rare but serious complication (less than 1% incidence). Can happen in any type but most common in RTSA. Clinical findings are important because infection becomes radiographically evident late in the course of disease. This might include progressive irregular lucency around the prosthesis. A multimodality approach including joint aspiration, cross-sectional imaging, and nuclear medicine studies, such as bone scintigraphy and indium labelled white blood cell radionuclide studies, is typically used to evaluate these patients.
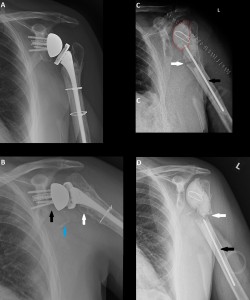
Fig 16: Anteroposterior (A)radiograph of a middle aged male, three years after a two-staged revision due to infection of previous left RTSA The patient reports persistent pain, however the radiograph shows no signs of complications. Aspiration was performed with negative cultures, in addition WBC and CRP were normal. Five years later, anteroposterior (B) radiograph demonstrates a new lucency at the glenoid and a gap between the scapula and glenosphere (black arrow), as well as a lucency at the humeral bone-cement interface (white arrow). A new curvilinear mineralization is present inferior to the joint (blue arrow). This was suspected for loosening + particle disease versus infection. A repeat aspiration resulted in positive culture for Cutibacterium Acnes (which is a low virulence infection). Post-revision anteroposterior (C) radiograph shows interval removal of RTSA and placement with a cement spacer (red line), a device that delivers antibiotics to the joint and stabilizes it while treating infection. Intramedullary nail was also inserted (black arrow) to treat a proximal humerus periprosthetic fracture the patient sustained before the surgery (white arrow). Follow-up anteroposterior radiograph (D) reveals inferior migration of the intramedullary nail with worsening alignment and medial translation of the distal humerus fragment.
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.
* Heterotopic ossification
Heterotopic bone formation following shoulder arthroplasty is frequent and develops early after surgery (45%),1 year after surgery. This is often low-grade without a functional significance, but when higher grade might limit range of motion.
* Misc.
Fig 17: An unusual case of an elderly female, 6 months after right RTSA. Anteroposterior (A) radiograph reveals a normal appearing prosthesis. There is however, an approximately rectangular lamellated object projected inferior to the glenoid and scapular neck (black arrows). The axillary view (B) shows that the location of this object is extra-articular, in the soft tissues near the scapula. Comparison with remote radiographs confirms that this object was present prior to the shoulder arthroplasty (C+D). It turned up to be a retained surgical sponge from a remote upper back lipoma removal.
Unpublished images: ©”Department of radiology, St. Joseph Hospital, London Ontario, Western Universiy/ Canada 2025”.