Retroperitoneal adenopathies are frequently encountered in clinical practice and can be associated with a wide range of both benign and malignant conditions. Accurate diagnosis is critical for guiding appropriate management, but the deep and complex anatomical location of retroperitoneal lymph nodes poses significant challenges for tissue sampling. Percutaneous biopsy, performed under image guidance, has emerged as a minimally invasive technique for obtaining diagnostic tissue while minimizing patient morbidity.
Technique
The retroperitoneal space is a complex anatomical region that can pose challenges when performing percutaneous biopsy of anatomical structures located in this area (Figure 1).
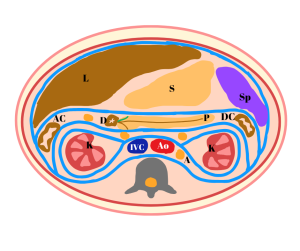
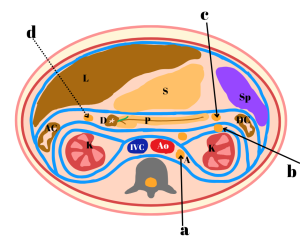
After evaluating the pre-procedural CT scan and performing an ultrasound assessment, the optimal access route is selected, primarily depending on the location of the adenopathy and its anatomical relationship with vital structures. The most commonly chosen approaches are the anterior transperitoneal or the retroperitoneal paravertebral routes.
When these approaches are not feasible, access to the adenopathy can also be achieved via a transhepatic route (avoiding the gallbladder, dilated bile ducts, and porta hepatis), transgastric, or transduodenal routes (Figure 2).
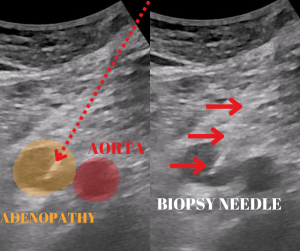
The choice of imaging modality for performing the percutaneous biopsy depends on the location of the adenopathy and whether ultrasound provides good visualization of the adenopathy, surrounding structures, and the biopsy needle's trajectory.
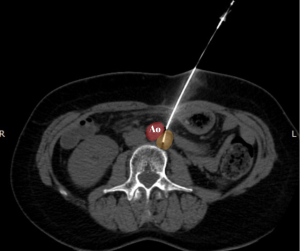
Computed tomography (CT) offers the advantage of better visualization of loco-regional anatomical structures, while ultrasound allows real-time visualization of the biopsy needle. A combined guidance approach using ultrasound and CT may be employed when the biopsy needle tip is difficult to identify solely under ultrasound guidance (Figure 3).
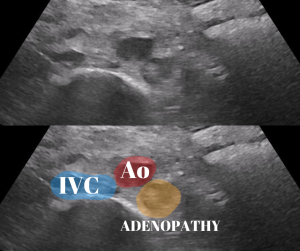
When ultrasound guidance makes biopsy needle localization difficult, CT examination can offer additional information and enhance procedural safety to minimize the risk of complications. (Figure 4).
Semi-automatic side-cutting biopsy needles (18G or 20G) are used in a coaxial system along with a coaxial trocar, enabling the collection of multiple biopsy fragments (Figure 5).
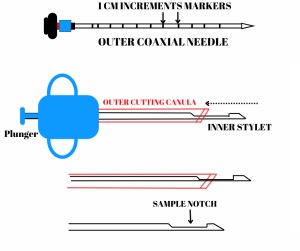
The choice of needle size is based on the selected pathway, the size of the adenopathy, and its proximity to vital structures, aiming to minimize the risk of complications.
Local anesthesia is administered using 1% lidocaine injected along the entire biopsy needle path.
Subsequently, the biopsy needle trocar is advanced to the adenopathy, followed by the insertion of the biopsy needle and the collection of tissue samples (Figure 6, Figure 7).