Unveiling the Inferior Vena Cava!
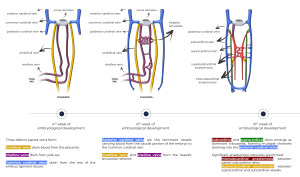
Embryology
The development of the inferior vena cava (IVC) involves a complex sequence of vascular formations, anastomoses, and regressions that occur between the 4th and 8th weeks of gestation.
In the 4th week of embryological development, three distinct paired veins are present: the umbilical veins, which drain blood from the placenta; the vitelline veins, which drain from the yolk sac; and the common cardinal veins, which drain the rest of the embryo's general tissue.
By the 6th week, the posterior cardinal veins become the dominant vessels, carrying blood from the caudal portion of the embryo to the common cardinal veins. The umbilical and vitelline veins contribute to the formation of the hepatic sinusoidal network.
Between the 6th and 8th weeks, the subcardinal and supracardinal veins emerge as dominant tributaries, forming multiple channels that drain into the posterior cardinal veins. This period also sees the formation of significant anastomotic networks, including the intersubcardinal anastomosis between the paired subcardinal veins and the suprasubcardinal anastomosis between the supracardinal and subcardinal vessels.
Anatomy
The IVC is typically formed by the confluence of the right and left common iliac veins behind the right common iliac artery at the level of the 5th lumbar vertebra. It ascends, receiving many tributaries, along the right side of the vertebral column, behind the duodenum, portal vein, and liver, before piercing the diaphragmatic central tendon at the caval opening at the level of the 8th thoracic vertebra. This is followed by a short intra-thoracic course before terminating at the right atrium.

Anomalies:
- Congenital absence
- Hypoplasia
- Pre-renal:
- Azygos continuation of the IVC (absent vitelline veins).
- Renal:
- Retroaortic left renal vein (persistent posterior supracardinal-subcardinal anastomisis).
- Circumaortic venous collar (persistent anterior and posterior supracardinal-subcardinal anastomosis).
- Post-renal:
- Transposition or left-sided IVC (persistent left supracardinal vein)
- Duplication of the IVC (persistent both supracardinal veins).
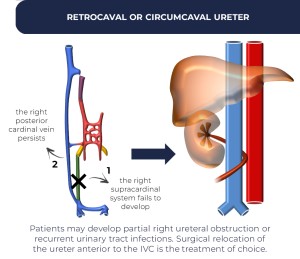
- Retrocaval or circumcaval ureter (persistent right posterior cardinal vein).
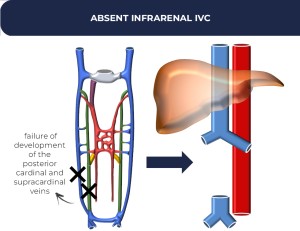
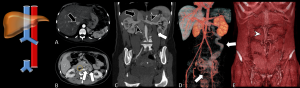
- Absent infrarenal segment (absent posterior cardinal and supracardinal veins).
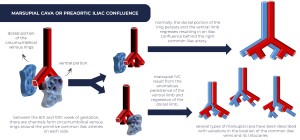
- Preaortic iliac confluence (marsupial cava).
A) Congenital absence:
Congenital absence of the IVC has an unknown incidence and unclear cause, as it is difficult to identify a single embryonic event. However, complete failure of embryonic vein development and sequelae of intrauterine or perinatal venous thrombosis with atrophy have been suggested as possible causes. Patients may experience symptoms of lower-extremity venous insufficiency or idiopathic deep venous thrombosis.
B) Hypoplasia
A rare congenital malformation that may be caused by embryological or acquired factors. It causes venous stasis, which increases the likelihood of venous thrombosis and collateral circulation.
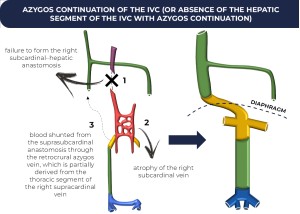
C) Azygos continuation of the IVC
In most cases, it is found incidentally, but there is an association with congenital heart disease, asplenia and polysplenia syndromes, as well as with duplication of the IVC. The sequence of events begins with the failure to form the right subcardinal–hepatic anastomosis with atrophy of the right subcardinal vein. As a result, blood is shunted through the suprasubcardinal anastomosis into the retrocrural azygos vein, which is partially derived from the thoracic segment of the right supracardinal vein.
It can cause an enlarged azygos vein. Care should be taken to avoid misdiagnosing it as a right-sided paratracheal mass or retrocrural adenopathy.
Preoperative knowledge may be important for planning cardiopulmonary bypass and to avoid difficulties in catheterizing the heart.
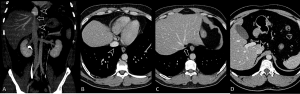
D) Retroaortic left renal vein
Persistence of the dorsal arch of the renal collar occurs in this variation, where the ventral arch (intersubcardinal anastomosis) regresses. As a result, a single left renal vein passes posterior to the aorta.
Remember that in conventional anatomy, the left renal vein (longer than the right renal vein) courses anteriorly to the abdominal aorta.
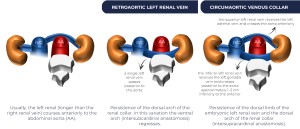

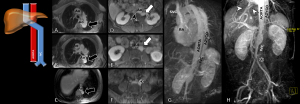
E) Circumaortic venous collar
Persistence of the dorsal limb of the embryonic left renal vein and the dorsal arch of the renal collar (intersupracardinal anastomosis). The superior left renal vein receives the left adrenal vein and crosses the aorta anteriorly. The inferior left renal vein receives the left gonadal vein and crosses posterior to the aorta approximately 1–2 cm inferiorly to the anterior.
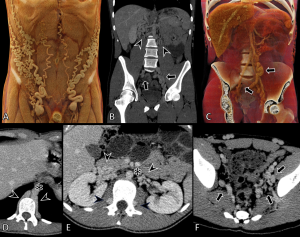
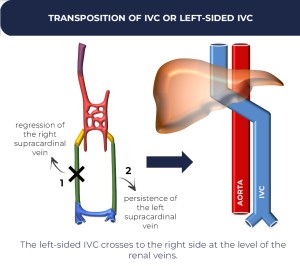
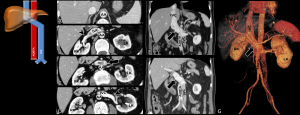
F) Transposition or left-sided IVC
It is the result of the regression of the right supracardinal vein and the persistence of the left supracardinal vein. The left-sided IVC crosses to the right side at the level of the renal veins.
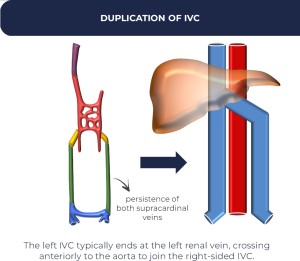
G) Duplication of the IVC
It results from the persistence of both supracardinal veins. The left IVC typically ends at the left renal vein, crossing anteriorly to the aorta to join the right-sided IVC.
H) Absent infrarenal segment
It results from the failure of development of the posterior cardinal and supracardinal veins.
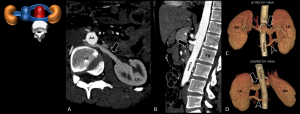
I) Retrocaval or circumcaval ureter
It results from the failure of the right supracardinal system to develop, while the right posterior cardinal vein persists. Patients may develop partial right ureteral obstruction or recurrent urinary tract infections. Surgical relocation of the ureter anterior to the IVC is the treatment of choice.

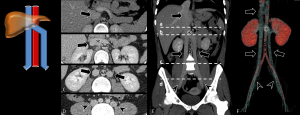
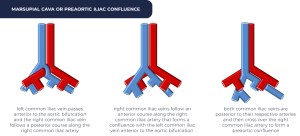
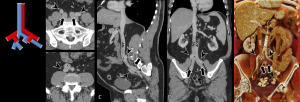
J) Preaortic iliac confluence (marsupial cava)
Between the 6th and 10th weeks of gestation, channels form circumumbilical venous rings around the primitive common iliac arteries on each side. Normally, the dorsal portion of the ring persists, and the ventral limb regresses, resulting in an iliac confluence behind the right common iliac artery.
Marsupial IVC results from the anomalous persistence of the ventral limb and regression of the dorsal limb. Several types of marsupial cava have been described, with variations in the location of the common iliac veins and their tributaries:
- The left common iliac vein passes anterior to the aortic bifurcation, and the right common iliac vein follows a posterior course along the right common iliac artery;
- The right common iliac vein follows an anterior course along the right common iliac artery, forming a confluence with the left common iliac vein anterior to the aortic bifurcation;
- Both common iliac veins are posterior to their respective arteries and then cross over the right common iliac artery to form a preaortic confluence.
Pitfalls
- Paracaval lipoma or pseudolipoma: volume-averaging artifact due to prominent pericaval fat above the caudate lobe rather than a true intraluminal lesion, more frequent in patients with chronic liver disease. It can mimic bland thrombus, spread of tumors, fat embolism and intracaval spread of renal angiomyolipoma. Multiplanar reconstructions confirm the true nature of this finding.
 Fig 22: Paracaval lipoma or pseudolipoma. Images from cardiac CT angiography (A, axial, B, coronal, C, sagittal) shows a band of adipose tissue (arrow) next to the IVC (arrowhead).
Fig 22: Paracaval lipoma or pseudolipoma. Images from cardiac CT angiography (A, axial, B, coronal, C, sagittal) shows a band of adipose tissue (arrow) next to the IVC (arrowhead). - Contrast flow phenomenon or pseudothrombosis.
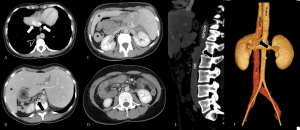
 Fig 23: Contrast flow phenomenon or pseudothrombosis. Images from chest CTA (A-C, axial, D, coronal, E, sagittal), an early phase dynamic scanning, show uniformly contrast enhanced blood in the renal veins (arrowhead) entering the IVC (arrows) when it is diluted by normal blood (without contrast) coming into the IVC from the pelvis and lower limbs (asterisk). This causes a swirl-like appearance. Later scans times allow contrast-enhanced blood to enter the lower limbs thus mixing evenly with the renal vein blood.
Fig 23: Contrast flow phenomenon or pseudothrombosis. Images from chest CTA (A-C, axial, D, coronal, E, sagittal), an early phase dynamic scanning, show uniformly contrast enhanced blood in the renal veins (arrowhead) entering the IVC (arrows) when it is diluted by normal blood (without contrast) coming into the IVC from the pelvis and lower limbs (asterisk). This causes a swirl-like appearance. Later scans times allow contrast-enhanced blood to enter the lower limbs thus mixing evenly with the renal vein blood. - Congenital malformations that drain into the IVC (increasing its flow and caliber) or vessels with similar pathways to the IVC may be potential confounding factors, such as anomalous pulmonary venous return and portosystemic shunts.
 Fig 23: Contrast flow phenomenon or pseudothrombosis. Images from chest CTA (A-C, axial, D, coronal, E, sagittal), an early phase dynamic scanning, show uniformly contrast enhanced blood in the renal veins (arrowhead) entering the IVC (arrows) when it is diluted by normal blood (without contrast) coming into the IVC from the pelvis and lower limbs (asterisk). This causes a swirl-like appearance. Later scans times allow contrast-enhanced blood to enter the lower limbs thus mixing evenly with the renal vein blood.
Fig 23: Contrast flow phenomenon or pseudothrombosis. Images from chest CTA (A-C, axial, D, coronal, E, sagittal), an early phase dynamic scanning, show uniformly contrast enhanced blood in the renal veins (arrowhead) entering the IVC (arrows) when it is diluted by normal blood (without contrast) coming into the IVC from the pelvis and lower limbs (asterisk). This causes a swirl-like appearance. Later scans times allow contrast-enhanced blood to enter the lower limbs thus mixing evenly with the renal vein blood. Fig 25: Infracardiac total anomalous pulmonary venous return. 11-day-old male neonate with cyanosis and tachypnea. Imagens from cardiac CT (A, coronal, B, C, axial maximum intensity projections, E, F, anterior and posterior three-dimensional volume-rendered reconstructions show the pulmonary veins draining through a single pulmonary venous trunk (SPVT). The pulmonary veins do not communicate with the hypoplastic left atrium (LA), descending to the infradiaphragmatic region and connecting to the portal vein (PV), resulting in a portal venous system aneurysm. An ostium secundum atrial septal defect (asterisk) and dilated right ventricle (RV) are observed. A = aorta, IVC = inferior vena cava, LIPV = left inferior pulmonary vein, LSPV = left superior pulmonary vein, LV = left ventricle, PV = portal vein, RA = right atrium, RIPV = right inferior pulmonary vein, RMPV = right middle pulmonary vein, RSPV = right superior pulmonary vein.
Fig 25: Infracardiac total anomalous pulmonary venous return. 11-day-old male neonate with cyanosis and tachypnea. Imagens from cardiac CT (A, coronal, B, C, axial maximum intensity projections, E, F, anterior and posterior three-dimensional volume-rendered reconstructions show the pulmonary veins draining through a single pulmonary venous trunk (SPVT). The pulmonary veins do not communicate with the hypoplastic left atrium (LA), descending to the infradiaphragmatic region and connecting to the portal vein (PV), resulting in a portal venous system aneurysm. An ostium secundum atrial septal defect (asterisk) and dilated right ventricle (RV) are observed. A = aorta, IVC = inferior vena cava, LIPV = left inferior pulmonary vein, LSPV = left superior pulmonary vein, LV = left ventricle, PV = portal vein, RA = right atrium, RIPV = right inferior pulmonary vein, RMPV = right middle pulmonary vein, RSPV = right superior pulmonary vein.