Reduction or interruption of intestinal blood flow, whether due to obstructive or non-obstructive causes, poses a risk of infarction, necrosis, and perforation of the bowel wall.Bowel ischemia accounts for 1-2% of abdominal pain cases in the emergency room and over 10% of acute abdomen cases in the elderly.Imaging is crucial, as early diagnosis is the only way to prevent the life-threatening outcomes of most ischemic events.The preferred diagnostic test is biphasic CT angiography of the upper abdomen and pelvis (arterial and venous phases). While unenhanced scans may provide additional information, they are not essential for diagnosis.Laboratory tests are often non-specific, except for lactate, which rises early and serves as a key marker of ischemia.
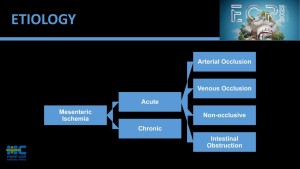
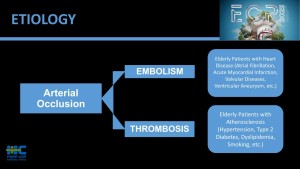
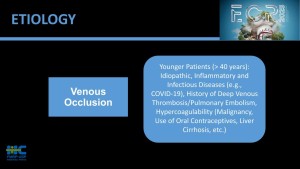
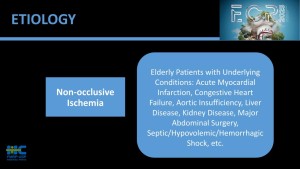
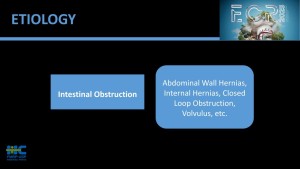
Figures 1 to 5 illustrate the types of ischemia and risk factors
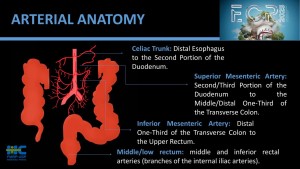
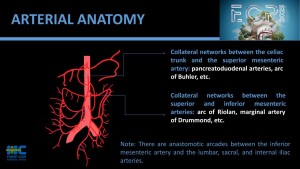
The arterial supply to the small bowel primarily stems from the superior mesenteric artery (SMA), which arises from the abdominal aorta just below the celiac trunk. The SMA gives rise to jejunal and ileal branches that supply the jejunum and ileum, forming arcades and vasa recta for efficient blood distribution. The proximal duodenum receives blood from the gastroduodenal artery (a branch of the common hepatic artery), while its distal portion is supplied by the inferior pancreaticoduodenal artery, a branch of the SMA. This dual supply ensures robust perfusion and collateral flow, crucial for maintaining small bowel function and integrity.
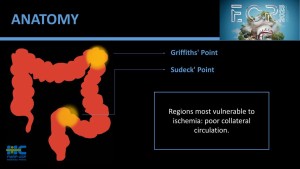
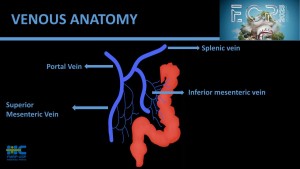
A description of arterial and venous supply and the so-called critical points is provided in figures 6 to 9
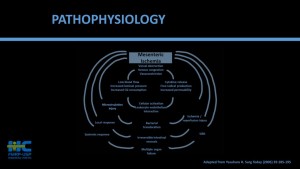
Also, the complex pathophysiology of intestinal ischemia is illustrated in figure 10