Breast phantom model preparation
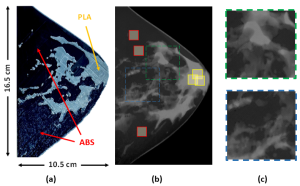
A digital compressed breast phantom (6.5 cm thick) obtained with breast CT [Zenodo Database [1], model number 1], with voxels classified as glandular tissue, adipose tissue and skin, were selected. The voxels of the compressed digital phantom are anisotropic, with 0.363 x 0.3663 mm2 resolution in planes parallel to the chest wall and 0.2663 mm along the nipple-to pectoral muscle direction. A craniocaudal slice (area: 10.5 x 16.5 cm2, thickness: 1.1 cm) was selected and exported as two STL files (one corresponding to gland and skin, and the other to fat, as shown in Fig. 1).
3D printing technique and material selection: Benchmark with commercial tissue-equivalent materials
FDM technology was selected for printing the physical breast slice, as it allows multi-material printing and there is a wide and versatile portfolio of filaments, which offer a wide range of radiological properties. A desktop printer BambuLab-X1C with 0.2mm nozzle and enclosed chamber was used.
After selecting filament materials with radiological properties similar to those of breast tissues [2], we compared their X-ray attenuation coefficients with reference breast tissue-equivalent materials [3] (CIRS 100% Gland and CIRS 100% Fat). It was concluded that PLA is a suitable substitute for glandular tissue and skin, and ABS, for adipose tissue. The selected filaments were ABS (navy blue, ρ = 1.05 g/cm3) and PLA (grey, ρ = 1.24 g/cm3).
3D printing conditions
First, several printing tests were carried out with the printer in the not default mode to obtain homogenous deposition of the material (avoid infill patterns on the images), avoid printing defects (warping, under extrusion, bad adhesion) and overcome incompatibilities between PLA and ABS due to their mechanical and thermal differences (clogged nozzle, extruder stuck). The suitable printing parameters that we found were 0.1mm layer height, 99% lines infill, 40 mm/s print speed, raft adhesion and chamber door semi-open, taking a printing time of 18 hours.
Physical evaluation of 3D printed phantom dimensions
The thickness of the printed phantom slice (shown in Fig. 2a) was measured at different points on its surface using a 0.05 mm resolution caliper. Visual inspection was also carried out to find possible printing defects.
Breast phantom evaluation in mammography
A Hologic 3Dimensions system was used to acquire 2D images of the breast slice, which was placed on the breast support table (using the compressor) in a position compatible with that of a real breast. Three for-processing images (an example shown in Fig. 2b) were acquired by manually selecting rhodium and silver filters combined with 29 kVp and 31 kVp, respectively. The three images were averaged, darkfield – flatfield corrected and the natural logarithm was applied. Mean pixel and standard deviation values were measured in three 1 x 1 cm2 ROIs placed on only fat or gland regions (Fig. 2b) that were selected based on the tissue distribution in the digital phantom slice from the Zenodo breast.
Effective X-ray attenuation coefficient calculation
The X-ray effective attenuation coefficient (µeff) was calculated by dividing the mean pixel value by the measured thickness. The µeff for each material was obtained by averaging the µeff values over each ROI set. These values were compared to those obtained for the reference breast tissue-equivalent materials. Their relative differences were computed for all the acquisition conditions.
Printing process quality evaluation and artifacts characterization: micro-CT imaging
The evaluation of printing quality and characterization of artifacts of the printed slice was performed based on micro-CT imaging (UCM Micro-CT Laboratory). The acquisition conditions were 50 kVp, 3 mAs, 1000 projections and X1.5 magnification. The reconstructed micro-CT volume (0.033 x 0.033 x 0.033 mm3 voxel size) was then segmented into PLA+ABS (voxel value = 1) and air (voxel value = 0).
The thickness of the printed phantom was obtained by summing the segmented slices of the volume and multiplying the resulting image by the thickness slice (0.033 mm). The relative differences between the thickness maps of the Zenodo and the micro-CT of the 3D-printed breast slices were calculated after aligning and reshaping both maps to have the same pixel size.