Results
Our preliminary findings reveal DDR shows a promising potential as a screening tool in patients with suspected pulmonary embolism. Initial analysis demonstrates encouraging diagnostic performance with a sensitivity of 54.55% (95% CI: 23.38–83.25%), indicating its capacity to identify a substantial proportion of patients with confirmed pulmonary embolism. The wide confidence interval underscores the ongoing nature of our investigation and the potential for improved performance with further optimization of acquisition and analysis protocols. Furthermore, DDR demonstrated a specificity of 66.67% (95% CI: 40.99–86.66%), correctly identifying a significant majority of patients without PE. These results suggest that DDR can effectively differentiate between patients with and without the condition. The observed positive likelihood ratio of 1.64 indicates that a positive DDR result modestly elevates the probability of PE, providing valuable information to clinicians. A negative likelihood ratio of 0.68, while suggesting a slight reduction in the likelihood of PE with a negative result, still contributes to the overall clinical picture when considered in conjunction with other diagnostic modalities.
Fig 6: Fig 6: [Fig 6 to Fig 9: Case no. 1] 69 year old male came with complains of acute breathlessness since 3-4 days with history of lower limb swelling. Screening TTE was normal. Patient was referred to radiology department for CTPA and a screening DDR was done which showed areas of hypoperfusion in bilateral mid zones (right> left). CTPA was done and showed multiple partially occluding eccentric filling defects in distal right and left pulmonary artery, their lobar, segmental and subsegmental branches, suggestive of bilateral pulmonary thromboembolism.
Fig 7: Fig 7: [Fig 6 to Fig 9: Case no. 1] 69 year old male came with complains of acute breathlessness since 3-4 days with history of lower limb swelling. Screening TTE was normal. Patient was referred to radiology department for CTPA and a screening DDR was done which showed areas of hypoperfusion in bilateral mid zones (right> left). CTPA was done and showed multiple partially occluding eccentric filling defects in distal right and left pulmonary artery, their lobar, segmental and subsegmental branches, suggestive of bilateral pulmonary thromboembolism.
Fig 8: Fig 8: [Fig 6 to Fig 9: Case no. 1] Patient was started on oral anticoagulants (Tab. Rivaroxaban 20mg) for management and came for a follow up. Follow DDR pulmonary perfusion map showed a significant improvement in pulmonary circulation in the previously affected region.
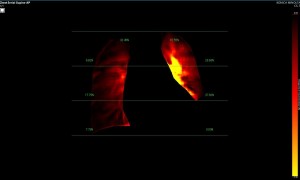
Fig 9: Fig 9: [Fig 6 to Fig 9: Case no. 1] Pulmonary perfusion summary mode: pre and post treatment. Significant improvement in pulmonary perfusion can be appreciated post treatment.
Fig 10: Fig 10: [Fig 10 to Fig 13: Case no. 2]: 44 year old male came with complains of breathlessness since 2 months, exaggerated since 2-3 days. Screening TTE was suggestive dilated RA and RV with RV systolic dysfunction. Patient had history of left thoracotomy done in year 2022 in view of pleural effusion.
Fig 11: Fig 11: [Fig 10 to Fig 13: Case no. 2] Patient was referred to radiology department for CTPA and a screening DDR was done. The left lower zone could not be assessed due to post thoracotomy status. However, even though left lower zone was not assessed, still the left side showed a better perfusion than right side, raising a suspicion of pathological perfusion in the right pulmonary circulation.
Fig 12: Fig 12: [Fig 10 to Fig 13: Case no. 2]: Pulmonary perfusion summary mode.
Fig 13: Fig 13: [Fig 10 to Fig 13: Case no. 2] CTPA was done and showed pulmonary thrombus in right pulmonary artery, extending into lower lobe segmental branches. Patient was started on oral anticoagulants (Tab. Rivaroxaban 20mg) and operative management is being planned for removal of thrombus.
Fig 14: Fig 14: [Fig 14 to Fig 16: Case no. 3] 33 year old male came with acute onset breathlessness since 4 hours. Screening TTE was normal. Patient was referred to radiology department for CTPA and a screening DDR was done which showed almost no perfusion in the right lung and an abnormal perfusion of the left lung.
Fig 15: Fig 15: [Fig 14 to Fig 16: Case no. 3]: Pulmonary perfusion summary mode.
Fig 16: Fig 16: [Fig 14 to Fig 16: Case no. 3]: CTPA was done and showed saddle thrombus in main pulmonary trunk extending into the right and left pulmonary artery with extension into the segmental and subsegmental branches of the right upper, mid and lower lobes and the left lower lobe.
Fig 17: Fig 17: [Fig 17 to Fig 20: Case no. 4]: A 36 year old female came with complains of sudden onset breathlessness since 1 day. Screening TTE was suggestive of dilated RA and RV. Patient was referred to radiology department for CTPA and a screening DDR was done which showed hypoperfusion of the right and hyperperfusion of the left lung.
Fig 18: Fig 18: [Fig 17 to Fig 20: Case no. 4]: Pulmonary perfusion summary mode.
Fig 19: Fig 19: [Fig 17 to Fig 20: Case no. 4]: CTPA was done and showed thromboemboli in right branch of pulmonary artery extending to all the right segmental branches and left interlobar artery. No distal contrast opacification on right side.
Fig 20: Fig 20: [Fig 17 to Fig 20: Case no. 4]: CTPA was suggestive of thromboemboli in right branch of pulmonary artery extending to all the right segmental branches and left interlobar artery. No distal contrast opacification on right side.