Congress:
ECR25
Poster Number:
C-10388
Type:
Poster: EPOS Radiologist (educational)
DOI:
10.26044/ecr2025/C-10388
Authorblock:
J. P. Coelho, S. Basso, H. Donato, A. Moreira, M. Sanches, M. J. Noruegas, P. J. V. Coelho, L. A. Ferreira, P. Donato; Coimbra/PT
Disclosures:
Joana Pinto Coelho:
Nothing to disclose
Susana Basso:
Nothing to disclose
Henrique Donato:
Nothing to disclose
Angela Moreira:
Nothing to disclose
Maria Sanches:
Nothing to disclose
Maria Jose Noruegas:
Nothing to disclose
Paulo José Vieira Coelho:
Nothing to disclose
Luis Amaral Ferreira:
Nothing to disclose
Paulo Donato:
Nothing to disclose
Keywords:
Gastrointestinal tract, Paediatric, Conventional radiography, Fluoroscopy, Ultrasound, Diagnostic procedure, Obstruction / Occlusion
Proximal Bowel Obstruction
1. ESOPHAGEAL ATRESIA
- Malformation in the separation of the primitive foregut into the trachea and esophagus [1]
- The most common type (78–90%) is characterized by a proximal esophageal pouch with a fistula between the trachea and distal esophagus [1]
- Clinical presentation:
- Excessive salivation
- Feeding intolerance
- Inability to pass a nasogastric tube (classic finding)
- Chest radiograph:
- Gaseous distention of the proximal esophageal pouch
- Coiling of the nasogastric tube within the pouch
- If there is a fistula between the trachea and distal esophagus, gas will be present in the distal bowel
- Treatment:
- Surgical repair and closure of the fistula
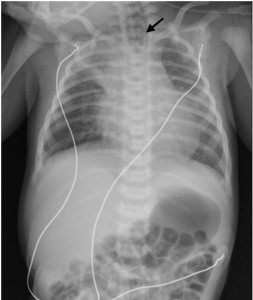
Fig 1: Anteroposterior radiograph of the chest in a 3-day-old female neonate who presented with difficulty passing a nasogastric tube shows the tip of the nasogastric tube (arrow) in the proximal esophageal pouch, indicating esophageal atresia, and gas is seen within the imaged gastrointestinal tract suggesting the presence of a distal tracheoesophageal fistula.
2. GASTRIC OR PYLORIC ATRESIA
- Often caused by a mucosal web in the region of the gastric antrum or pylorus [1]
- Clinical presentation:
- Non-bilious vomiting within the first hours of life
- Abdominal radiograph:
- Single bubble sign (dilatation of the stomach)
- Absence of gas distal to the pylorus
- Treatment:
- Surgical repair
3. HYPERTROPHIC PYLORIC STENOSIS
- Thickening of the muscular layer of the pylorus and its failure to relax [2]
- Clinical presentation:
- Projectile non-bilious vomiting
- If it progresses further, a palpable pyloric mass ("olive") may be detected
- Abdominal radiograph (non-specific):
- Normal
- Single bubble sign with distal gas
- Caterpillar sign - stomach wall indentations due to gastric hyperperistalsis against a closed pylorus
- Abdominal ultrasound:
- Hypoechoic thickening of the muscular layer of the pylorus >3 mm
- Pyloric channel length >12–16 mm
- Minimal or absent gastric emptying during study
- Treatment:
- Pyloromyotomy

Fig 2: Hypertrophic pyloric stenosis in a 23-day-old male neonate presented with projectile nonbilious emesis and abdominal distension. Abdominal ultrasound reveals a thickening of the pyloric muscle that measures 5 mm and the pyloric channel is elongated and measures 19 mm.
4. DUODENAL ATRESIA
- Failure of the duodenal lumen recanalization during embryonic development, leading to a blind-loop duodenum [1]
- Prenatal diagnosis (50% of cases): [3]
- Double bubble sign (dilatation of the stomach and proximal duodenum)
- Polyhydramnios
- Clinical presentation:
- Bilious vomiting within the first hours of life
- Failure to pass meconium
- Abdominal radiograph (diagnostic):
- Double bubble sign
- Absence of distal gas
- Treatment:
- Surgical repair
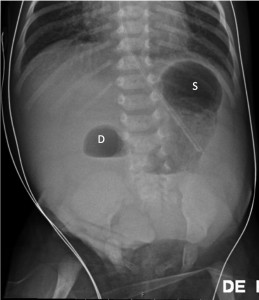
Fig 3: Anteroposterior abdominal radiograph in a 0-day-old female neonate with suspected duodenal atresia on prenatal ultrasound demonstrating the double bubble sign with air distended stomach (S) and a dilated proximal duodenum (D) with absent distal bowel gas, suggesting duodenal atresia.
5. ANNULAR PANCREAS
- During embryonic development, the ventral pancreatic bud fails to rotate normally, and a rim of pancreatic tissue surrounds the second part of the duodenum [1]
- Clinical presentation:
- Bilious vomiting
- Abdominal radiograph:
- Double bubble sign
- Presence or absence of distal gas, depending on the degree of the obstruction (severe cases may mimic duodenal atresia)
- Abdominal ultrasound:
- Abnormal pancreatic tissue surrounding the duodenum
- Treatment:
- Surgical repair
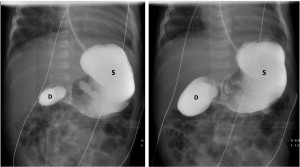
Fig 4: A 12-day-old female neonate with vomiting and suspected duodenal atresia on prenatal ultrasound, but with a normal radiograph of the chest at birth. Image from an upper gastrointestinal contrast study shows dilatation of the stomach (S) and proximal duodenum (D) with a filiform passage of the contrast agent into the nondilated distal bowel. During surgery, an annular pancreas was found.
6. DUODENAL WEB
- A membrane across the duodenal lumen with a central hole. Long-term pressure of peristalsis against the stenotic segment of the duodenum may lead to distal stretching of the web, forming an intraluminal pseudodiverticulum [4]
- Clinical presentation:
- Bilious vomiting
- Abdominal radiograph:
- Double bubble sign
- Presence of distal gas (due to decompression through the central hole)
- Variable dilatation over serial radiographs due to intermittent decompression through the central hole
- Abdominal ultrasound:
- Gas and/or fluid-filled diverticulum at the junction of the second and third duodenal portions
- Collapse of the third portion of the duodenum
- Exclusion of malrotation with volvulus
- Upper gastrointestinal contrast study:
- Distension of the stomach and proximal duodenum
- Duodenal diverticulum at the junction of the second and third portions
- When contrast agent passes through the central hole, it forms a curvilinear filling defect with contrast agent appearing in the nondilated distal duodenum – “windsock” sign
- Treatment:
- Surgical repair
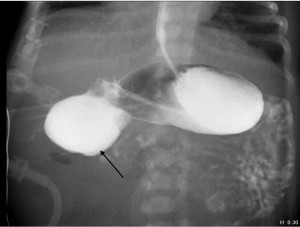
Fig 5: Duodenal web in a 1-day-old male neonate with vomiting. Image from an upper gastrointestinal contrast study shows dilatation of the stomach and proximal duodenum. The contrast agent has passed through the central hole of the web into the nondistended duodenum, outlining the web as a curvilinear filling defect, the so-called windsock sign (arrow).
7. MALROTATION WITH MIDGUT VOLVULUS
- Abnormal embryologic rotation and fixation of the intestinal tract can lead to malposition of the ligament of Treitz, causing narrowing of the mesenteric root and predisposing to intestinal volvulus, leading to intestinal ischemia, infarction, and necrosis [1]
- Clinical presentation:
- Bilious vomiting
- Abdominal radiograph:
- Normal or nonspecific
- Double bubble sign with distal gas
- Single bubble sign with distal gas
- Abdominal ultrasound:
- Abnormal superior mesenteric artery (SMA)-superior mesenteric vein (SMV) relationship:
- The SMV lies to the left of the aorta-SMA axis (seen in 47% of cases)
- A normal SMA-SMV relationship may be present in up to 30% of patients with malrotation!
- Abnormal position of the third portion of the duodenum:
- Normal rotation: the third portion crosses the midline between the aorta and SMA (meaning it is retroperitoneal)
- Malrotation: the duodenum is abnormally intraperitoneal and, if complicated by volvulus, its third portion passes anteriorly to the SMA before incorporating into the volvulus
- Whirlpool sign - the most specific ultrasound sign and identifies the volved portion
- Abnormal superior mesenteric artery (SMA)-superior mesenteric vein (SMV) relationship:
- Upper gastrointestinal contrast study (if ultrasound is inconclusive):
- Dilatation of stomach and proximal duodenum
- Abnormal duodenojejunal junction position:
- Normally, it should cross to the left of the spine and ascend to the duodenal bulb level
- In malrotation, the junction does not cross the midline, remaining on the right
- Corkscrew sign - twisting pattern indicative of volvulus
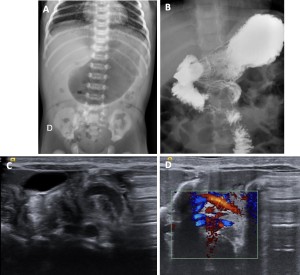
Fig 6: A 5-day-old male neonate presented with bilious emesis. (A) Anteroposterior abdominal radiograph shows a dilated gas-filled stomach with some gas seen distally, resulting in a single bubble with distal gas appearance. (B) Image from an upper gastrointestinal contrast study shows a corkscrew appearance of the distal duodenum and jejunum, representing the midgut volvulus. Ultrasound without (C) and with (D) color Doppler was performed, revealing the whirlpool sign of midgut volvulus.
8. JEJUNAL ATRESIA
- Ischemic insult in utero [1]
- Clinical presentation:
- Vomiting
- Abdominal distension
- Failure to pass meconium
- Abdominal radiograph (diagnostic):
- Triple bubble sign (dilatation of stomach, duodenum, and jejunum)
- Absence of distal gas
- Treatment:
- Surgical repair
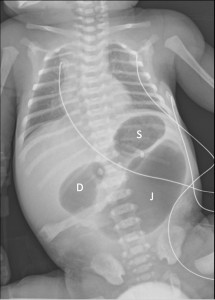
Fig 7: Anteroposterior radiograph of the chest in a 2-day-old female newborn with jejunal atresia who presented with abdominal distension and vomiting shows the triple bubble sign with 3 distended air-filled bubbles, including the stomach (S), duodenum (D), and jejunum (J) with lack of distal bowel gas.
Distal bowel obstruction
9. ILEAL ATRESIA
- Ischemic insult in utero [1]
- Clinical presentation:
- Vomiting
- Abdominal distension
- Failure to pass meconium
- Abdominal radiograph:
- Multiple dilated loops of bowel (low obstruction pattern)
- Absence of distal gas
- May have massive focal dilatation of a loop of bowel
- Contrast enema:
- Microcolon
- Passage of contrast agent retrogradely into the ileum and stopping at the level of the atresia
- Dilated loops of unopacified bowel proximal to the point of atresia
- Treatment:
- Surgical repair

Fig 8: Ileal atresia in a 1-day-old female neonate with bilious vomiting and abdominal distension. Anteroposterior abdominal radiograph shows diffuse dilatation of loops of bowel. No gas is seen within the rectum.
10. MECONIUM ILEUS
- Presence of inspissated meconium lodged in the distal ileum, causing obstruction [1]
- Up to 80% of cases are associated with cystic fibrosis [1]
- Clinical presentation:
- Bilious vomiting
- Abdominal distension
- Failure to pass meconium
- Abdominal radiograph:
- Multiple dilated bowel loops with absence of distal gas
- Absence of air-fluid levels on lateral view (due to thick inspissated meconium)
- Mottled (“soap bubble”) appearance of loops of bowel due to air mixed with meconium
- Contrast enema:
- Microcolon (difficult to distinguish from ileal atresia)
- Filling defects within opacified terminal ileum (distinguishes from ileal atresia)
- Dilated loops of unopacified bowel proximal to the terminal ileum
- Treatment:
- Serial enemas with N-acetylcysteine
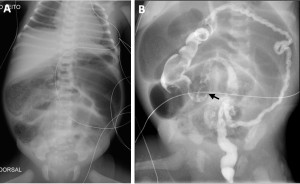
Fig 9: A 2-day-old newborn girl presented with abdominal distension. (A) Anteroposterior abdominal radiograph shows diffuse dilatation of loops of bowel. A mottled appearance is noted involving loops of bowel which is the “soap bubble” appearance. (B) Contrast enema shows a microcolon. In the distal ileum, there are multiple small rounded filling defects (arrow), representing inspissated meconium.
11. COLONIC ATRESIA
- Typically affects the colon proximal to the splenic flexure
- Clinical presentation:
- Abdominal distension
- Failure to pass meconium
- Abdominal radiograph:
- Multiple dilated loops of bowel with absence of distal gas
- May have massive focal dilatation of a loop of bowel
- Contrast enema:
- Microcolon up to the level of atresia
- May show characteristic kink in colon at the site of atresia
- Dilated loops of unopacified bowel proximal to the point of atresia
- Treatment:
- Surgical repair
- Rectal biopsy is necessary due to association with Hirschsprung disease!
12. HIRSCHSPRUNG DISEASE
- Absence of normal neuronal cells in the submucosal and myenteric plexus of the large bowel, causing functional intestinal obstruction [5]
- Short-segment disease (75%) is the most common type
- Clinical presentation:
- Abdominal distension
- Failure to pass meconium within 48 hours
- Abdominal radiograph:
- Diffuse bowel dilatation
- Absence of gas within rectum (but the presence does not exclude the diagnosis!)
- Contrast enema (short-segment disease):
- Transition point at the rectosigmoid junction
- Reversed rectosigmoid ratio:
- Affected segment is narrowed due to increased tone (normally, the rectum is wider than the sigmoid)
- Corkscrew configuration and irregular appearance of mucosa of the aganglionic segment
- Dilated loops of bowel proximal to the transition point
- Contrast enema (long segment disease):
- Similar appearance, but the transition point is at a more proximal location
- The rectosigmoid ratio can be normal, but the caliber of the involved distal colon is smaller than that of the proximal colon
- Contrast enema (total colonic disease):
- The entire colon has a narrow caliber, with the appearance of a “pseudomicrocolon” (similar to ileal atresia or meconium ileus)
- A definitive diagnosis requires rectal biopsy
- Treatment:
- Surgical repair
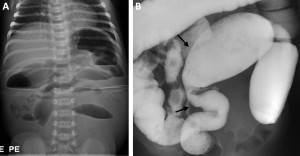
Fig 10: Hirschsprung disease in a 10-day-old male neonate with abdominal distention and delayed passage of meconium. (A) Anteroposterior abdominal radiograph shows multiple dilatation of loops of bowel suggesting a distal bowel obstruction. (B) Contrast enema demonstrates greater luminal distension of the sigmoid compared with the rectum (arrows).
13. FUNCTIONAL IMMATURITY OF THE LARGE BOWEL
- A benign, usually self-limiting, transient, functional colonic obstruction due to immature neuronal cells in the myenteric plexus [5]
- Most common cause of delayed meconium passage within the first 48 hours of life.
- Clinical presentation:
- Abdominal distension
- Delayed passage of meconium
- Abdominal radiograph:
- Multiple dilated loops of bowel (similar to Hirschsprung disease)
- Contrast enema:
- Normal rectosigmoid ratio
- Caliber of left colon smaller than caliber of right colon
- Gradual caliber change in the region of splenic flexure
- Multiple filling defects throughout colon (meconium plugs)
- Dilated loops of bowel proximal to the caliber change
- Passage of meconium plugs immediately after the study, leading to clinical improvement
- Treatment:
- Conservative management

Fig 11: A flowchart that provides a structured diagnostic approach for neonates presenting with suspected bowel obstruction.