We present five cases illustrating the diverse variations of superior vena cava anomalies, along with associated cardiac, venous, and aortic abnormalities, and discuss their clinical implications.
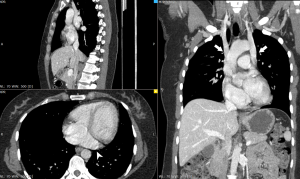
Case I: A 44-year-old male presented with headaches, a recent history of cerebral stroke, and paroxysmal supraventricular tachycardia. Thoracic CT angiography (CTA) revealed duplication of the superior vena cava (SVC), with the right SVC draining into the left atrium, as evidenced by paradoxical filling of the left heart chambers, while the left SVC drained into an enlarged coronary venous sinus. Additionally, a right superior lobar pulmonary vein was observed draining into the right SVC. The patient was discharged with recommendations for radiofrequency ablation and appropriate medical management.

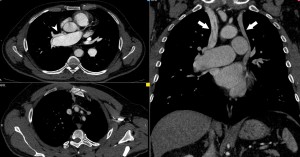
Case II:
A 55-year-old woman was referred to the cardiology department for further investigation of pulmonary hypertension. Asymptomatic for cardiac issues, she had a recent history of cerebral stroke. Transesophageal echocardiography identified an atrial septal defect-type sinus venosus with a left-to-right shunt and coronary venous sinus dilatation. Thoracic CT angiography revealed SVC duplication, with the persistence of left brachiocephalic vein. Additionally, a right superior lobar pulmonary vein drained into the right SVC. She was subsequently referred to the cardiothoracic surgery team for repair of the septal defect and correction of the anomalous venous return.

Case III: A 41-year-old male with a history of surgically corrected aortic coarctation presented with acute cardiac insufficiency. EKG showed atrial flutter, and echocardiography revealed a low left ventricular ejection fraction and a hypoechoic mass in the right atrium, raising suspicion for an intracardiac thrombus. Thoracic CTA excluded thrombosis but identified focal occlusion of the descending aorta with an anastomosis between the left subclavian artery and the descending aorta, along with retrograde aortic opacification. It also showed SVC duplication, agenesis of the hepatic segment of the inferior vena cava, and a dominant hemiazygos vein draining into the left SVC. Cardioversion restored sinus rhythm, and cardiac MRI was recommended for further evaluation.
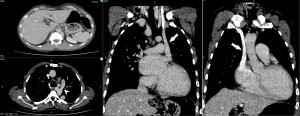

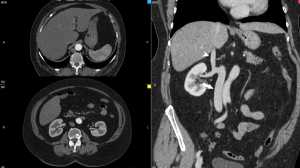
Case IV:
A 65-year-old woman presented with dyspnea and palpitations, associated with paroxysmal atrial fibrillation and left ventricular insufficiency. An ablation procedure for atrial fibrillation was attempted but was unsuccessful due to the inability to access the right atrium with the catheters. This raised suspicion of inferior vena cava agenesis, prompting the performance of a thoracic CTA. The CTA revealed a persistent left SVC and agenesis of the right SVC, along with agenesis of the infrarenal segment of the inferior vena cava, and an ascending lumbar vein on the right of the aorta. The patient was discharged with careful cardiological monitoring and optimal medical management.
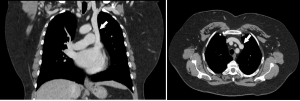
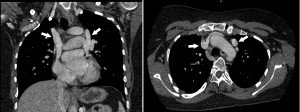
Case V: A 26-year-old woman was admitted for follow-up investigations with a history of aortic coarctation, Turner syndrome, horseshoe kidney, and sinus tachycardia. Thoracic CTA revealed duplication of the SVC with a persistent left brachiocephalic vein, aortic coarctation in the isthmic segment (postductal) with post-stenotic dilation, a horseshoe kidney, a bovine aortic arch, and a Lusoria artery (left subclavian artery with a retro-esophageal course). Given the patient's current condition, surgical intervention was not indicated, and she was recommended for ongoing monitoring.

In summary, among the five patients presented, four exhibited arrhythmias, one of whom had a venous return anomaly suspected after an invasive procedure failed. Two cases were associated with aortic coarctation, one with an atrial septal defect, and none were asymptomatic at presentation. These findings highlight the diverse clinical presentations of SVC anomalies, which radiologists may encounter in both symptomatic and asymptomatic patients. The presence of associated congenital pathologies should always be considered in the diagnostic process. The cases discussed emphasize the importance of not only identifying the various types of SVC anomalies but also understanding their clinical implications in order to guide appropriate management.