According to the revised Atlanta classification, the morphological imaging findings of acute pancreatitis are stratified into 2 main categories: interstitial edematous pancreatitis and necrotizing pancreatitis.
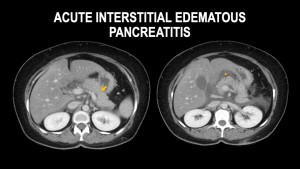
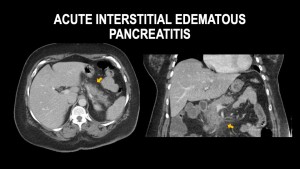
- Interstitial edematous pancreatitis (IEP)
IEP is more common and represents non necrotizing inflammation of the pancreas. On contrast enhanced CT the imaging features include:
- Pancreas appears diffusely enlarged due to inflammatory edema.
- The parenchyma demonstrates homogenous enhancement, occasionally it might be less avid, however with absence of pancreatic or peri-pancreatic necrosis.
- The peri-pancreatic fat may show fat stranding and/or peripancreatic fluid commonly in the anterior pararenal space.
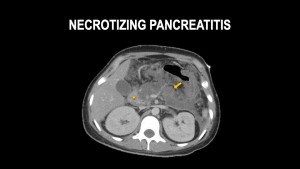
- Necrotizing Pancreatitis:
It is less common, seen in 5 – 10 % of patients presenting with acute pancreatitis. It is due to impaired perfusion of the pancreas and or peripancreatic tissues.
It is differentiated into three patterns based on the location of necrosis into: pancreatic (5%), peripancreatic (20%) or combined (75%). The imaging findings include:
- Pancreatic: focal or diffuse non-enhancement of the pancreatic parenchyma without the presence of a peripancreatic necrotic collection.
- Peri-pancreatic: diffuse pancreatic enhancement however with heterogenous, mixed, collection(s) in the peripancreatic tissues.
- Combined necrotizing pancreatitis: Focal or diffuse non enhancing areas involving the pancreatic parenchyma associated with adjacent necrotic peripancreatic collections.
Fluid Collections in Acute Pancreatitis:
Over time, acute pancreatitis may form fluid collection(s), which according to revised Atlanta Classification System are categorized depending on the type of pancreatitis (IEP vs Necrotizing) and duration since onset of symptoms.

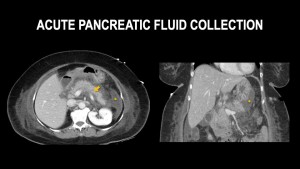
- Acute Peri-pancreatic Fluid Collection (APFC):
Occurs during the first 4 weeks of IEP. When present APFC will often resolve or may progress to pseudocyst. It’s imaging features include:
- Homogenous fluid attenuation collections in the peripancreatic region.
- Absence of well-defined walls and solid components within the collection.
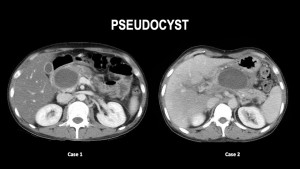
- Pseudocyst:
Occurs more than 4 weeks after symptom onset in IEP. It occurs when APFCs has not resolved and becomes more organized resulting in an encapsulated collection. It is seen in approximately 10% of IEP cases, and approximately 25% of patients develop symptoms or infection which necessitates intervention. It’s Imaging features include:
- Well circumscribed collection with an enhancing wall.
- Homogenous fluid attenuation collection with absence of nonliquefied/ solid components.
- Typically, peripancreatic in location.
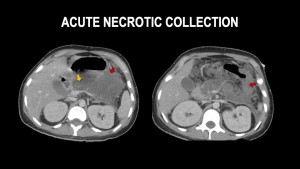
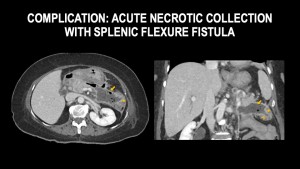
- Acute Necrotic Collection (ANC):
Occurs within the first 4 weeks of symptoms onset in necrotizing pancreatitis. It represents non encapsulated necrotic collections. It's Imaging features include:
- Presence of pancreatic necrosis (focal or diffuse areas of hypo enhancing pancreatic parenchyma)
- Heterogenous, ill-defined and poorly organized collection
- Presence of nonliquefied debris within the collection, such as solid-appearing components or fat globules within the fluid.
- Frequently large in size
- Collection may be pancreatic, peri-pancreatic or combined.
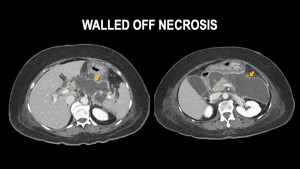
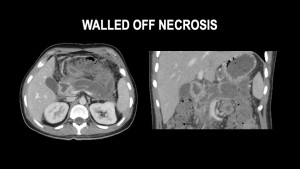
- Walled Off Necrosis (WON):
Occurs after 4 weeks of symptoms onset in necrotizing pancreatitis. It represents encapsulated necrotic collections. It's imaging features include:
- Heterogenous collection containing nonliquefied debris within the fluid.
- Thick enhancing wall
- Collection may be pancreatic, peri-pancreatic or combined.
Complications of Acute Pancreatitis:
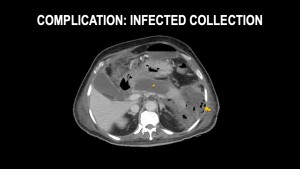
1. Infected Collection
Infection is a complication in approximately 20% of patients with necrotizing pancreatitis and is believed to stem from bacterial translocation from the gut to the necrotic pancreatic tissue. The most frequently identified bacteria include Escherichia coli, Staphylococcus aureus, and Enterococcus faecalis, though other microorganisms may also be present. While infection can develop at any stage of the disease, it is most commonly observed between two to four weeks after the initial presentation. The main imaging finding of an infected collection is the presence of gas within the collection.
2. Pancreatic-enteric fistula
Necrotic collections can erode through the bowel wall, most commonly in the colon and duodenum resulting in pancreatic-enteric fistulas. It presents with gas bubbles within the collections secondary to the fistula. It more commonly occurs infected collections.
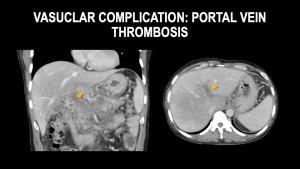
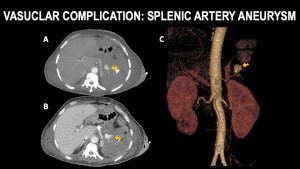
3. Vascular Complications:
These arise due to an inflammatory response, which can lead to splenic vein thrombosis—the most frequently observed vascular complication—while the superior mesenteric and portal veins are less commonly affected. They also occur due to erosion of blood vessels secondary to release of pancreatic enzymes, potentially leading to spontaneous arterial bleeding or the formation of pseudoaneurysms.