PELVIC INFLAMATORY DISEASE (PID)
PID is an infection affecting the upper female genital tract, including the endometrium, fallopian tubes, and ovaries. It is commonly associated with sexually transmitted infections or iatrogenic causes. Endometritis most frequently occurs during pregnancy or postpartum.
Typical symptoms include lower abdominal pain, vaginal discharge, fever, and dyspareunia.
PID primarily affects women of reproductive age and, if left untreated, it may lead to long-term complications such as infertility, ectopic pregnancy, and chronic pelvic pain.
Ultrasound is the preferred initial imaging modality. CT can assist in determining disease extension, associated complications, and providing further assessment in patients unresponsive to antibiotic therapy. Additionally, when facing nonspecific symptoms, CT is frequently used, allowing evaluation of a broader range of conditions.
Imaging findings:
Early in the stages of infection, US and CT findings may be normal.
- Cervicitis/endometritis (early stages of infection):
- Enlarged cervix, hyperemic endocervical canal, parametrial fat stranding/ hyperechogenicity.
- Enlarged uterus, fluid in the uterine cavity, abnormal endometrial enhancement and indistinct uterine border.
- Free fluid might be present.
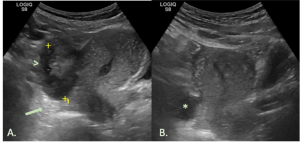
- Salpingitis/pyosalpinx
- Tubal tortuosity, wall hyperemia and tubal thickening.
- Complex internal fluid within a dilated tube.
- Adjacent pelvic edema, fat stranding/hyperechogenicity and free fluid.
- MR imaging is a more sensitive modality for identifying ovarian involvement.
- Tubo-ovarian abscess (late stage of infection):
- Multilocular septate cystic adnexal mass, with a thick and enhancing wall.
- Loss of fat planes between the mass and the adjacent pelvic structures.
- Thickening of the uterosacral ligaments.
- Free fluid might be present.

ADNEXAL TORSION
Adnexal torsion represents approximately 2.7% of gynecological surgical emergencies. It occurs when adnexal structures - including the ovary, the fallopian tube or even a paraovarian cyst - undergo twisting around the infundibulopelvic and utero-ovarian ligaments, compromising the ovarian artery, vein and lymphatic channels, leading to vascular congestion and potential ischemia.
Premenopausal women are the most commonly affected group, often due to a benign adnexal mass serving as the lead point for the torsion. Although less frequent, torsion can also occur in normal ovaries, mainly in prepubertal girls.
The primary symptom is pelvic pain, often accompanied by nausea and vomiting. As the clinical presentation is vague and nonspecific, this diagnosis is frequently delayed or initially overlooked.
Imaging findings:
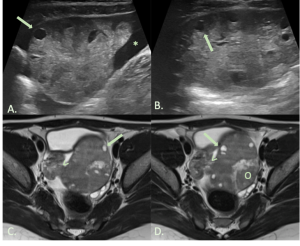
- Asymmetric ovarian enlargement (largest diameter >5cm when no ovarian lesion is present).
- Thickened ovarian parenchyma surrounding a lesion.
- Peripheral follicle displacement – “string of pearls” sign.
- Hyperechoic rim surrounding the follicles at US – “follicular ring” sign.
- Twisted pedicle and whirlpool sign.
- Parenchymal edema and hemorrhage related changes: hypoechoic areas or heterogeneity at US, increased attenuation at non-contrast CT, increased T1 (hemorrhage) and T2 (edema) weighted signal intensity at MRI.
- Tilting of the uterus toward the affected side and abnormal location of the ovary.
- Free pelvic fluid.
- Presence of flow at Doppler study does not exclude torsion!
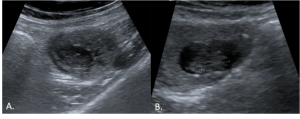
HEMORRAGIC OVARIAN CYST
A hemorrhagic ovarian cyst may be a physiologic and self-limited event that involves a follicular cyst or corpus luteum. However, significant hemorrhage can lead to abrupt onset of pelvic pain and, if there is cyst rupture, it may result in a life-threatening situation due to associated hemoperitoneum and hypotension.
The exact mechanism behind luteal cyst rupture remains unclear, although the increased vascularity of the ovary during the luteal phase likely increases the risk of rupture.
On imaging, the primary differential diagnosis is ectopic pregnancy, making correlation with β-HCG levels is essential.
Imaging findings:
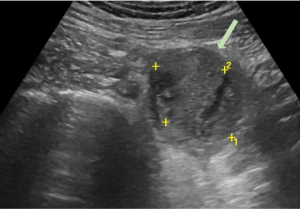
- The US appearance varies depending on the age of the hemorrhage and the clot formation. Typical features include a low-level echogenic adnexal cyst with a lace-like internal pattern.
- On CT, findings include an adnexal cyst with high attenuation areas (>40 HU) within the lesion.
- The MRI imaging appearance also depends on hemorrhage’s stage. Lesions may appear hyperintense on both T1- and T2-weighted images or hyperintense on T1- and hypointense on T2-weighted images.
- After cystic rupture, hemoperitoneum can be observed. In some cases, contrast-enhanced CT can show active contrast extravasation adjacent to the cyst, indicating ongoing bleeding.
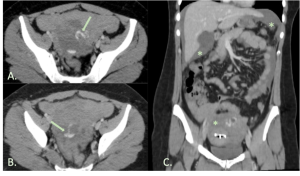
RUPTURED ECTOPIC PREGNANCY
Ectopic pregnancies occur when the blastocyst implants outside the endometrium of the uterus. Most ectopic pregnancies (approximately 95%) occur in the fallopian tube, particularly in the ampullary region. Major risk factors include a previous ectopic pregnancy, tubal surgery, and pelvic inflammatory disease.
A high index of suspicion for ectopic pregnancy should always be maintained in patients presenting with pelvic pain and elevated β-hCG levels.
Rupture of an ectopic pregnancy is a life-threatening situation as it can lead to significant hemorrhage. Hypovolemic shock and shoulder pain (secondary to diaphragmatic irritation) are indirect signs that may suggest rupture.
Ultrasound is the primary imaging modality to determine whether a pregnancy is intrauterine or ectopic. Although CT is usually not the imaging technique of choice in a known pregnant patient, it may be used for evaluation of a severe acute abdomen without prior ultrasound. MRI may be useful in hemodynamically and clinically stable patients requiring additional information to guide therapeutic decisions.
Imaging findings:
- No evidence of intrauterine pregnancy.
- Adnexal cystic sac-like structure that is separate from an ipsilateral normal ovary, representing a potential gestational sac.
- A moderate-to-large amount of free pelvic fluid or hemoperitoneum, seen on any imaging modality, particularly when associated with a poorly defined, complex adnexal mass, should always raise suspicion of a ruptured ectopic pregnancy.
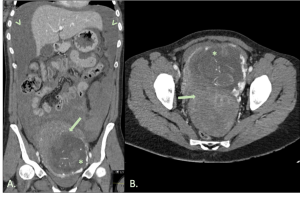
UTERINE RUPTURE
Uterine rupture is a rare but potentially catastrophic pregnancy complication, involving a complete tear through of all three uterine layers (endometrium, myometrium and perimetrium). Most cases occur in the setting of a trial of labor after cesarean delivery, though it has been reported in non-pregnant women due to trauma, infection, or malignancy. Clinically, it usually presents with hemodynamic instability and abdominal pain.
Uterine dehiscence is a similar condition, characterized by an incomplete tear that does not penetrate all uterine layers, and is often an incidental finding in an asymptomatic patient.
Uterine perforation represents another serious condition that can complicate any type of intrauterine procedure or implantation.
These terms are sometimes used interchangeably.
Ultrasound is the initial imaging technique of choice, CT may be selectively utilized to further assess or clarify findings and MRI serves as a problem-solving tool when prior imaging results are inconclusive, while clinical suspicion of remains high.
Imaging findings:
- Visualization of a protruding segment of the amniotic sac.
- Fetal parts within the peritoneal cavity.
- Uterine wall defect.
- Extrauterine hematoma.
- Free fluid or hemoperitoneum.
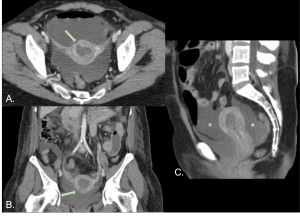
OVARIAN VEIN THROMBOSIS (OVT)
OVT is most commonly observed in postpartum patients, particularly after cesarean delivery. However, it can also develop as a complication following pelvic surgery, pelvic trauma or complicate other disorders such as pelvic inflammatory disease or chemotherapy. The right ovarian vein is predominantly affected, accounting for approximately 80-90% of cases.
OVT may lead to serious complications, including sepsis and thrombus extension to the inferior vena cava or left renal vein and, though rare, pulmonary embolism.
Clinical presentation includes fever and lower abdominal pain, but it can also remain asymptomatic, particularly in postpartum patients or following major gynecological surgeries.
Imaging findings:
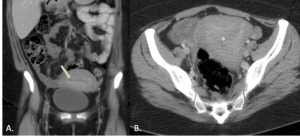
The diagnosis can be made using ultrasound, however, CT provides clearer visualization.
- On ultrasound, a tubular or serpiginous hypoechoic structure may be identified in the adnexa, near the ovarian artery. If the ovarian vein is visualized, the absence of Doppler flow can be useful.
- On CT, typical features include a tubular structure with a thickened enhancing wall and a central low-attenuation thrombus, located in the expected course of the ovarian vein.
- These findings should be carefully differentiated from conditions such as hydroureter, acute appendicitis, or thrombosis of the inferior mesenteric vein.
