Tuberous sclerosis complex (TSC) is a genetic neurocutaneous disorder (or phacomatosis) with autosomal dominant inheritance that predisposes to benign tumor formation (hamartomas) in a wide range of organs - brain, kidneys, skin, heart, lungs. It is caused by a mutation in either of two genes, TSC1 or TSC2, which are related to hamartin and tuberin production respectively. The former and the latter play an important role as tumor growth suppressors and regulate cell proliferation and differentiation. Loss of function of the hamartin-tuberin complex leads to cell growth stimulation and, therefore, an immensely diverse clinical presentation in patients - from mild disease to severe multisystem features.
Despite the genetic predisposition, the mutation can often occur spontaneously, with most cases presenting sporadically. TSC has an estimated incidence of 1 in 6000 to 1 in 12,000 individuals, where the TSC 2 gene mutation accounts for more a severe clinical course.
In most patients TSC is diagnosed in childhood or infancy. The (Vogt) triad of clinical signs (seizures, intellectual disability, facial angiofibromas) is pathognomonic for TS, leading to a presentation of seizures, intellectual and developmental delay. Nevertheless, this characteristic clinical course occurs in less than 50% of the cases and since TSC can affect many areas and organs, causing an extensive variability of symptoms, this may lead to misinterpretations and delay in diagnosis and management. For this reason, a multidisciplinary approach is essential, including clinical evaluation, imaging techniques and genetic testing, with radiological studies playing a crucial part in recognizing the diagnostic criteria, treatment decision making and follow-up of these patients.
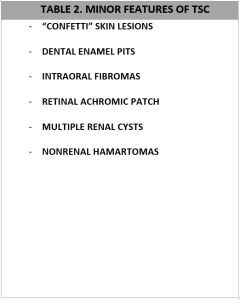
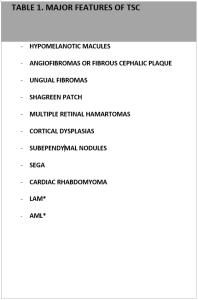
Since the last update in 2012, the International TSC Consensus Group categorizes the clinical manifestation of TSC into major and minor features.