In this section, we focused on clinical cases from our institution and illustrate the MR features of some of the most frequent congenital cardiac diseases:
Tetralogy of Fallot (TOF):
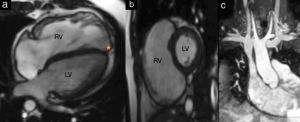
Fig. 7: Cardiac MRI in a 28-year-old patient with pulmonary regurgitation after repair of TOF with transannular patch repair. a-b. 4 chamber view cine imaging with enlarged right ventricle (RV) and normal sized left ventricle (LV). The apex is formed by the RV (orange star) while in a normally sized heart, it is formed by the LV. c. coronal cine TrueFISP MRI view demonstrates mild dilatation of the RVOT at the site of transannular patch.
References: Department of Pediatric Radiology, Medical University of Graz, Austria
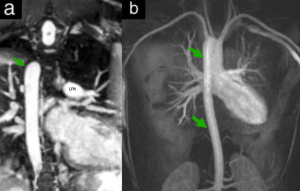
Fig. 8: a-b. Follow-up of a repaired TOF of a 21-year-old patient. MR-Angiography: TOF with associated right descending aorta (25 %) (green arrows). LPA = left pulmonary artery.
References: Department of Pediatric Radiology, Medical University of Graz, Austria
Transposition of the great arteries (TGA):
Transposition of the great arteries TGA is the second most common cyanotic heart defect after TOF.
The arterial switch operation can be associated with stenosis of the pulmonary artery, supravalvular stenosis of the aorta or pulmonary artery, aortic root dilatation, aortic valve regurgitation or coronary problems.
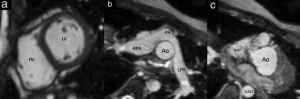
Fig. 9: TGA after arterial switch operation.
a. Cine SSFP sequence for evaluation of volume and function of the ventricles. b-c. MR-angiography of the main vessels: pulmonary artery is brought anterior of the ascending aorta and the LPA and RPA “flow” around the AAO. PA= pulmonary artery, AAO= ascending aorta, DAO= descending aorta, SVC= superior vena cava, RV= right ventricle, LV= left ventricle.
References: Department of Pediatric Radiology, Medical University of Graz, Austria
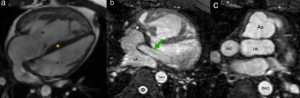
Fig. 10: TGA after atrial switch operation with Mustard procedure.
a. Cine MRI 4-chamber view: The RV is hypertrophied and positioned anteriorly; the LV is smaller and has less myocardial mass. The septum (orange star) tends to pertrude into the LV due to increased RV pressure. b. Baffle view in TGA after Mustard procedure with baffle from the SVC and IVC to the mitral valve (green arrow). LA= left atrium. c. The aorta is positioned anteriorly and arises from the hypertrophied, morphologically RV. The pulmonary artery is positioned posteriorly and arises from the LV.
References: Department of Pediatric Radiology, Medical University of Graz, Austria
Coarctation of aorta (CoA):
Coarctation of the aorta can be discrete, affecting the aortic isthmus, or diffuse, causing hypoplasia of the transverse arch. Atypical forms may involve stenosis extending into the descending aorta or dysplastic changes in the aortic arch.
CMR provides a detailed evaluation of the narrowing's extent, the condition of the head and neck arteries, and the collateral blood flow.
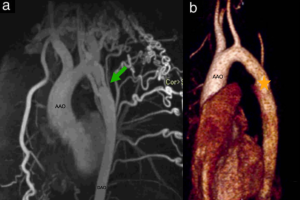
Fig. 11: a. 20-year-old pacient with history of coarctation repair at 4 years of age. MR-Angiography (MRA) shows mild recurrent narrowing at the isthmus (green arrow) and multiple subclavian and intercostal collaterals inserting into the descending aorta (DAO) distal to stenosis. b. VR 3D reconstruction of aorta after surgical resection of aortic coarctation and end-to-end anastomosis (orange star). AAO = ascending aorta.
References: Department of Pediatric Radiology, Medical University of Graz, Austria
Patent ductus arteriosus (PDA):
Aortic arch anomalies arise from abnormal fusion and regression of the branchial arches during embryologic development, affecting the aortic arch, pulmonary arteries, and ductus arteriosus. CMR offers detailed anatomical visualization and can also identify associated airway abnormalities.
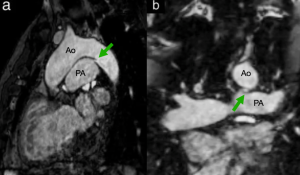
Fig. 12: Native cardiac MR angiography in a 11-year-old patient for pre-surgical assessment in sagittal (a) and coronal (b) planes demonstrates a persistent connection between the descending aorta and pulmonary artery (green arrows), consistent with Patent Ductus Arteriosus. Ao= aorta. PA= pulmonary artery.
References: Department of Pediatric Radiology, Medical University of Graz, Austria
Atrial septal defect (ASD):
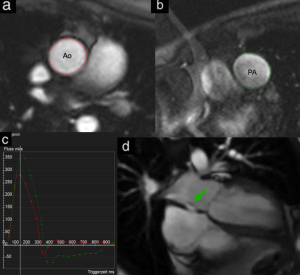
Fig. 13: a-b. Phase-contrast MRI images of the ascending aorta (Ao, red contour) and pulmonary artery (PA, green contour) used for blood flow quantification. c. Flow-time graphic showing blood flow in the aorta (red) and pulmonary artery (green). The pulmonary artery exhibits a higher peak flow, while the aortic flow shows a brief negative component, indicating retrograde flow due to shunting. d. Cine cardiac MRI demonstrating the presence of a right-to-left shunt (green arrow) across the interatrial septum.
Ventricular septal defect (VSD):
Ventricular septal defects are classified based on their location within the ventricular septum. The most common type, perimembranous VSDs (70%), involve a defect in the left ventricular outflow tract.
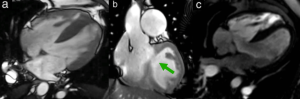
Fig.14: a-c.Enhanced cardiac MR-angiography showing a perimembranous VSD (green arrow).
References: Department of Pediatric Radiology, Medical University of Graz, Austria
Univentricular heart - Fontan circulation:
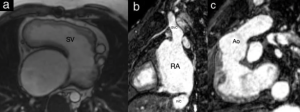
Fig. 15: SSFP cine MRI in axial (a) and sagittal (b-c) planes demonstrating an univentricular heart with a single ventricular chamber (SV). Fontan circulation. RA= right atrium, SVC= superior vena cava, IVC= inferior vena cava.
Congenital valve defects:
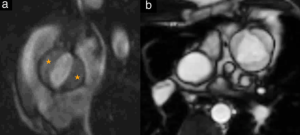
Fig. 16: a. Axial cine MRI depicting a bicuspid aortic valve (orange stars), characterized by two instead of three leaflets, which can lead to valve dysfunction. b. Cine SSFP sequences of a normal tricuspid aortic valve, serving as a reference for comparison.
Hypertrophic cardiomyopathy (HCM):
Cardiovascular MRI is a valuable tool for diagnosing HCM and monitoring patients after surgical myomectomy or septal ablation. Additionally, MRI can help distinguish HCM from other cardiomyopathies and cardiac conditions.
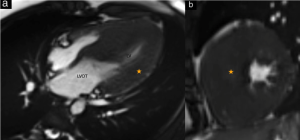
Fig.17: a-b. Case of a 16-year-old patient with hypertrophic cardiomyopathy and left ventricular outflow tract obstruction. Severe left ventricle wall hypertrophy (orange stars). The MRI was performed for op-planning and therapy monitoring. RV= right ventricle. LVOT= left ventricular outflow tract.
References: Department of Pediatric Radiology, Medical University of Graz, Austria