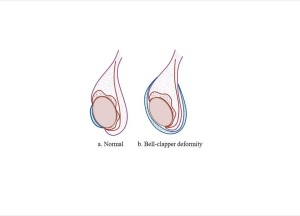
Testicular torsion represents a common surgical emergency. Therefore, early diagnosis and prompt surgical treatment are pivotal.There are two types of testicular torsion, the intravaginal and the extravaginal [1]. The age distribution in pediatric patients has a bimodal pattern: the extravaginal one occuring from the prenatal or perinatal period to the first year of life and the intravaginal one affecting boys older than 12 years old [1]. The most frequent type is the intravaginal one, where spermatic cord torsion is located within the tunica vaginalis [2]. Intravaginal torsion is attributed to bell clapper deformity of tunica vaginalis, which is usually present bilaterally [1, 2].
Generally, the degree of spermatic cord torsion varies from 90° to 1080° [3]. Regarding the degree of torsion, complete, partial, or intermittent testicular torsion can arise.
- Complete torsion is defined as a degree of spermatic cord twist of 360° or greater, which commonly causes abruption of intratesticular blood flow [1].
- Partial torsion occurs when the affected testis rotates less than 360°; hence, the perfusion of testicular parenchyma is usually preserved [1].
- Intermittent torsion or Torsion-detorsion syndrome refers to recurrent episodes of acute testicular pain followed by spontaneous resolution due to detorsion [4].
The degree of spermatic cord twist is critical for testicular viability, as a tight 720° torsion can lead to necrosis in a four-hour interval [1]. However, in cases of partial or intermittent torsion a twisted testis can be viable after several days [1].
Testicular torsion mainly presents with sudden unilateral testicular pain, sometimes along with nausea, low-grade fever [1, 4]. In cases of partial torsion, the clinical presentation is often atypical with subtle symptoms, whereas in intermittent torsion spontaneous regression of symptoms is noted [2]. Physical exam reveals asymmetric scrotum enlargement with a swollen, tender, erythematous hemi-scrotum [3]. A high-riding testicle or horizontal testicular lie can be also present [3, 4]. Absence of the cremasteric reflex is the most sensitive clinical sign [5, 6]. Negative Prehn’s sign is also noted (when elevating the testes, pain does not resolve) [3].
Clinical manifestations of this entity are often nonspecific; thus, an ultrasound exam allows the Paediatric Radiologist to safely narrow down the differential diagnosis of acute scrotum.