ANATOMY
The extratesticular space encompasses structures such as:
- Scrotal wall: Comprised of skin, dartos muscle, external spermatic fascia, cremasteric fascia and internal spermatic fascia. Except for dartos, these components extend centrally to join the spermatic cord.
- Tunica vaginalis: Formed by the testes' embryonic descent through the abdominal wall as a sock-like peritoneal evagination.
- Epididymis: A highly coiled, epithelial-lined tube surrounded by smooth muscle.
- Tunica albuginea: A fibrous covering of the testis that extends posteriorly, forming the mediastinum testis.
- Spermatic cord: Comprising three arteries (testicular, deferential, cremasteric), three nerves (genital branch of the genitofemoral, cremasteric nerve, sympathetic nerve fibers), three fasciae (external spermatic fascia, cremasteric fascia, internal spermatic fascia), ductus deferens, pampiniform plexus and lymphatic vessels.
Loose connective tissue is also present within the paratesticular space, composed of extracellular matrix and cellular components such as fibroblasts, myofibroblasts and adipocytes. Consequently, the extratesticular scrotum histologically consists of various epithelial, mesothelial, and mesenchymal elements.
IMAGING EVALUATION
The primary imaging modality for scrotal disease is ultrasound. Typically, high-frequency transducers are used. To ensure a comprehensive evaluation, it is imperative not only to focus on the testicles but also to explore the paratesticular tissues. If a palpable lump is present, confirming that a sonographic finding corresponds to the palpable area of concern is critical. Lastly, Doppler evaluation is an essential part of the examination. Magnetic resonance imaging is reserved for the few sonographically indeterminate cases.
EXTRATESTICULAR SCROTAL MASSES AND PSEUDOMASSES BY ANATOMICAL COMPARTMENTS
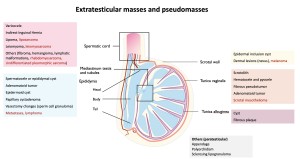
Organizing extratesticular scrotal masses and pseudomasses according to their anatomic compartments can be useful for narrowing the differential diagnoses (figure 1):
I. Scrotal wall
- Epidermal inclusion cyst
-
- Origin: Epidermal inclusion cyst is a common benign epithelial cyst that arises from the implantation of the infundibulum of a hair follicle. It is also referred to as an epidermoid, sebaceous or infundibular cyst, with the term "sebaceous cyst" considered a misnomer.
- Clinical features: Typically presents as a firm, slow-growing mass. It can become inflamed and/or infected.
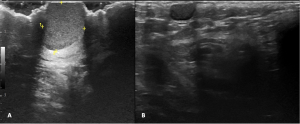
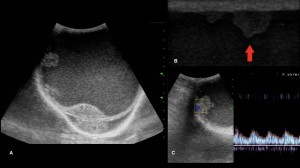
- Imaging features: Characterized by a well-circumscribed lesion with dermal attachment, avascular nature, increased acoustic transmission, and varying internal echogenic material (fig. 2). The presence of a tract connecting the cyst to the skin surface is considered pathognomonic.
- Treatment: If clinically bothersome, surgical excision with preservation of the cyst wall may be performed.
II. Tunica Vaginalis
- Scrotolith
- Origin: Unclear – it may result from torsion of the testicular/epididymal appendix, hematoma or inflammation of the tunica vaginalis.
- Clinical features: Asymptomatic or tender upon palpation.
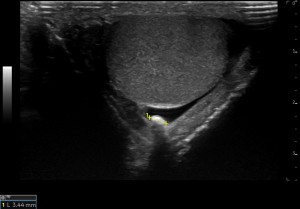
- Imaging features: Hyperechoic focus with a discrete acoustic shadow, located between the layers of the tunica vaginalis (fig. 3). It is freely mobile in the presence of a hydrocele.
- Treatment: none
- Hematocele and pyocele
-
- Origin: Collections of fluid in the potential space of the tunica vaginalis, that are complicated by hemorrhage or infection.
- Clinical features are essential for establishing a diagnosis:
- Hematocele is typically associated with trauma.
- Pyocele presents with acute scrotal pain, fever, dysuria and thickening of the scrotal skin.
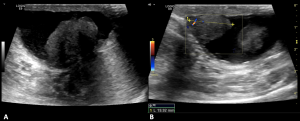
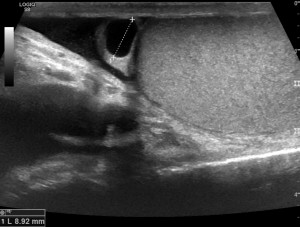
- Imaging features: Complex collections with internal echoes and septations (fig. 4). Pyoceles may exhibit hyperechoic foci and shadowing compatible with gas. When the pyocele progresses into a scrotal abscess, a well-demarcated hyperemic wall around the purulent fluid collection is evident.
- Treatment:
- Hematocele: Drainage may be necessary for large hematoceles.
- Pyocele: Most cases respond well to antibiotic therapy.

- Fibrous pseudotumor
- Origin: Arises from the tunica and represents a benign fibroinflammatory reaction, typically secondary to infection, trauma or surgery; possible association with IgG4-related disease.
- Clinical features: scrotal fullness or discomfort, often accompanied by a history of trauma.
- Imaging features: Characterized by one or more solid tumors, typically a hypoechoic mass with posterior acoustic shadowing (fig. 5).
- Treatment: excision if symptomatic.
- Scrotal mesothelioma
- Origin: Rare tumor that arises from malignant transformation of mesothelial cells in the tunica vaginalis, that may infiltrate local soft tissues and metastasize to retroperitoneal lymph nodes. Risk factors include asbestos exposure, chronic hydrocele, trauma, radiation and recurrent epididymitis.
- Clinical features: Painless scrotal enlargement.
- Imaging features: Hydrocele and nodular or plaquelike hypervascular lesions along the tunica vaginalis (fig. 6). Mesothelioma should be considered in the setting of a rapidly growing hydrocele.
- Treatment: Radical orchiectomy.
III. Epididymis and tubular system
- Spermatocele or epididymal cyst
- Origin: These are the most common extratesticular lesions, and their high prevalence accounts for why most of extratesticular lesions are benign. A spermatocele is a retention cyst occurring in the head of the epididymis that contains nonviable sperm, while an epididymal cyst is of lymphatic origin and contains serous fluid.
- Clinical features: Palpable lesion.
- Imaging features: Frequently they are sonographically indistinguishable. A spermatocele appears as a simple or minimally complex cystic lesion with low-level echoes, known as the "falling snow" sign, and acoustic streaming on Doppler imaging. An epididymal cyst is anechoic and has a thin wall (fig. 7).
- Treatment: Conservative.
- Adenomatoid tumor
- Origin: It is a benign tumor, the most common solid epididymal lesion, believed to originate from mesothelial cells. It typically arises in the tail of the epididymis but can also involve the tunica vaginalis and spermatic cord.
- Clinical features: Asymptomatic or painless scrotal mass among among patients aged 20-50 years.
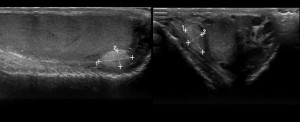
- Imaging features: Well-circumscribed oval mass, often hypovascular or avascular, typically slightly hyperechoic with refractive edge shadows, arising from the tail of epididymis (fig. 8 and 9).
- Treatment: Options include excision, biopsy and surveillance.
- Epidermoid cyst
- Origin: A benign tumor composed exclusively of ectoderm derivatives and presenting as a solid nodule due to keratinized contents. While most epidermoid cysts are intratesticular, they can also originate from the epididymis.
- Clinical features: Non tender, palpable lump.
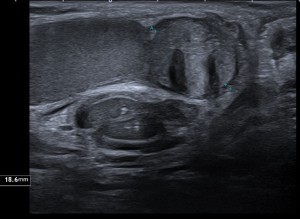
- Imaging features: Classic lamellated or “onion skin” appearance, avascular (fig. 10).
- Treatment: Conservative.
- Papillary cystadenoma
- Origin: It is thought to arise within the efferent ductules of the epipidymal head and can occur associated with von Hippel-Lindau disease, especially when they are bilateral.
- Imaging features: May appear solid due to tiny cystic spaces or be predominantly cystic.
- Treatment: Active surveillance.
- Metastases, lymphoma
- Malignancies of the epididymis are rare but can occur in the form of lymphoma and metastatic disease.
- Imaging features: These lesions should be considered when a solid mass concomitantly involves the intra and extratesticular space. Concomitant involvement occurs more often with lymphoma than with germ cell tumors. However, infectious and inflammatory processes, such as sarcoidosis and tuberculosis, may involve both regions and mimic malignancy.
IV. Tunica Albuginea
At this level, two types of pseudomasses should be recognized:
- Cyst
- Clinical features: Very firm and easily palpable.
- Imaging features: Sharply demarcated simple cyst on the surface of the testis (fig. 11).
- Fibrous plaque
- Origin: May result from previous episodes of trauma or infection.
- Imaging features: Hyperechoic thickening of the tunica, sometimes exhibiting calcification (fig. 12).
V. Spermatic Cord
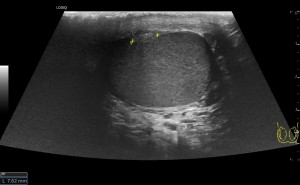
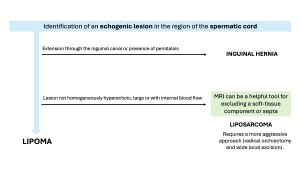
Suspicion for malignancy must be particularly higher at the level of the spermatic cord. Spermatic cord lipoma is considered one of the most common extratesticular neoplasms and can sometimes be misinterpreted as a fat-containing inguinal hernia. When lipoma is ruled out, the incidence of malignancy substantially increases (fig. 13).
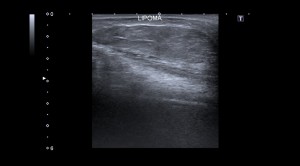
- Lipoma
- Origin: Benign collection of adipocytes unavailable for systemic metabolism
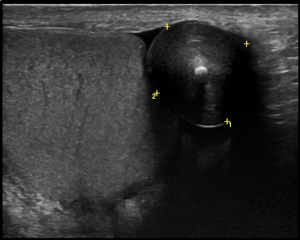
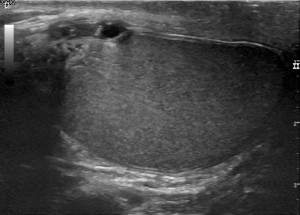
- Imaging features: Well-defined homogeneously hyperechoic mass, mostly avascular (fig. 14).
-
- Differential diagnoses
- Indirect inguinal hernia
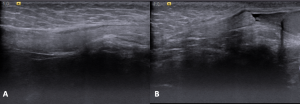
- Extension of intra-abdominal structures through the deep inguinal ring, demonstrating movement with the Valsalva maneuver (fig. 15). Bowel-containing hernias may show peristalsis.
- Indirect inguinal hernia
- Differential diagnoses
-
-
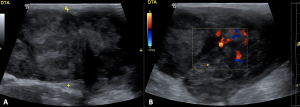
- Liposarcoma
- Malignant counterpart of lipoma, typically seen in men in 5th-7th decades.
- Variable appearance based on the relative amount of fat and soft-tissue components. It is often heterogeneously echogenic with areas of hypoechogenicity (fig. 16).
- Requires radical orchiectomy.
- Liposarcoma
-
-
-
- Other benign lesions and sarcomas
-