ENOSTOSIS
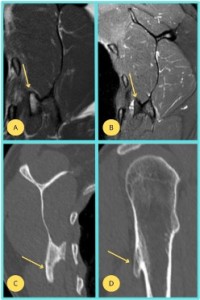
Typically appears as a small, well-defined, radiodense lesion located within the trabecular bone, often in the proximal femur or pelvis. It is important to differentiate it from more aggressive lesions, and its appearance is best seen on CT, which shows the lesion’s endosteal location and the preservation of cortical integrity (17, 18).

OSTEOID OSTEOMA
Usually presenting in the long bones, is characterized by a small, central nidus surrounded by a sclerotic zone, best visualized on CT scans. On MRI, the nidus may show up as a focal area of low signal intensity, while the surrounding sclerosis appears as a high-signal zone (1).

SUBCHONDRAL CYSTS
Offten associated with degenerative joint diseases and present as fluid-filled cavities beneath the articular cartilage, usually seen on plain X-rays or MRI. Their well-demarcated, radiolucent appearance can help distinguish them from more aggressive lesions like bone tumors (5).
FIBROUS DYSPLASIA
This condition involves replacement of normal bone with fibrous tissue, demonstrates a characteristic "ground-glass" appearance on both X-rays and CT scans. MRI may show heterogeneous signal intensity, reflecting the fibrous and osseous components (1).


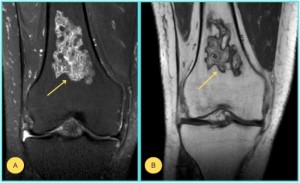
CHONDROMYXOID FIBROMA
It is a rare benign cartilaginous tumor that typically appears as a lobulated, well-defined, radiolucent lesion on X-ray, often in the metaphysis of long bones. On MRI, it shows mixed low and intermediate signal intensity with peripheral enhancement after contrast. A multimodal imaging approach is crucial for accurate diagnosis, allowing for detailed evaluation of the lesion's size, location, and characteristics, helping to distinguish it from more aggressive bone pathologies (2).

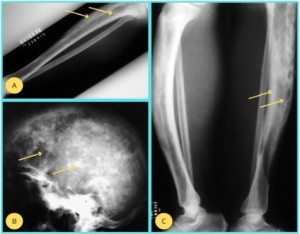
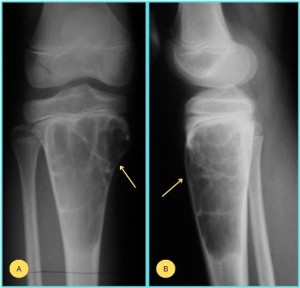
NON-OSSIFYING FIBROMA (NOF)
Typically found in the metaphysis of long bones in children and adolescents, is characterized by a well-defined, eccentric, radiolucent lesion with a thin sclerotic rim on X-ray. CT scans demonstrate a cystic lesion with a trabecular bone appearance and minimal to no periosteal reaction, which helps distinguish it from malignant lesions (1, 2).

OSSIFYING FIBROMA
It is more common in the craniofacial bones, presents as a well-circumscribed, expansile lesion with varying degrees of ossification. On CT, it demonstrates a mixed-density pattern with both radiolucent and radiopaque areas, and on MRI, it shows low-to-intermediate signal intensity with peripheral enhancement (10).

CORTICAL FIBROUS DEFECTS
These lesions are usually asymptomatic and present as small, oval or round, radiolucent lesions with a sclerotic border, often found in the distal femur or proximal tibia. These defects are typically smaller than NOF and lack the expansile nature of ossifying fibroma, making them easily distinguishable on imaging (11, 12).

SIMPLE BONE CYSTS (SBC)
SBC are fluid-filled lesions that appear as well-circumscribed, radiolucent areas in the metaphysis of long bones, commonly in the proximal humerus or femur. On X-ray, they may demonstrate a "fallen fragment sign", where a fragment of bone is displaced within the cystic space. CT and MRI provide further clarity, with MRI showing a well-defined cyst with low signal intensity on T1 WI and high signal intensity on T2 WI (1, 2).

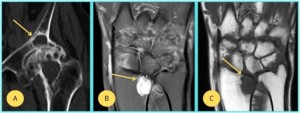
ANEURYSMAL BONE CYSTS (ABCs)
Expansile lesions with a characteristic multilocular appearance and a "bubbly" or "soap-bubble-like" pattern visible on X-ray or CT. On MRI, ABCs are hyperintense on T2-weighted images, with internal septations and peripheral rim enhancement after contrast administration, which helps differentiate them from other cystic lesions (1, 2).
BONE INFARCTS
Bone infarcts are typically seen in the femoral head, are often the result of ischemia and present with a subchondral lucency and crescent sign on X-ray, indicating collapse of the bone structure. CT and MRI are more sensitive, revealing areas of necrosis with an irregular border and low signal intensity on T1-WI and high signal intensity on T2 WI (2).
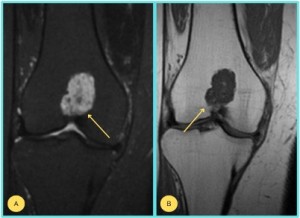
ENCHONDROMAS
Benign cartilage lesions which typically appear as radiolucent areas with calcified, ring-like or stippled patterns within the lesion on X-ray. CT reveals a lobulated mass with areas of calcification, while MRI shows intermediate signal intensity on T1 and high signal intensity on T2, reflecting the cartilaginous content (1-3).

CALCIFYING CHONDROMAS
Rare benign cartilage tumors that present as well-defined, radiolucent lesions with calcification in the central portion, visible on X-ray. On CT, they demonstrate a mixture of calcified and non-calcified areas, and MRI shows a heterogeneous signal intensity, with regions of low signal intensity due to calcifications (1-3).

OSTEOCHONDROMAS
One of the most common benign bone tumors, appear as bony exostoses with a cartilage cap, seen on X-ray as a sessile or pedunculated growth extending from the cortical surface. MRI is particularly useful in assessing the thickness of the cartilage cap, as an abnormal increase in thickness may suggest malignant transformation (2).
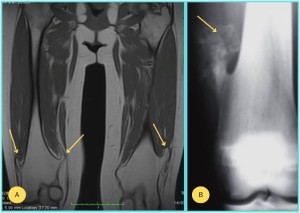
MULTIPLE HEREDITARY EXOSTOSES (MHE)
MHE is an autosomal dominant condition that presents with multiple osteochondromas scattered throughout the skeleton, most often in the metaphyses of long bones. These lesions appear as multiple bony protrusions on X-ray, with cartilage caps visible on MRI. The pattern of lesion distribution and the presence of a cartilage cap are key to diagnosing MHE and distinguishing it from solitary osteochondromas (2, 16).
MELORHEOSTOSIS
Melorheostosis is a rare sclerosing bone disorder, typically seen on radiographs with a "flowing" or "dripping candle-wax" appearance, where cortical sclerosis extends along the bone shaft. X-rays show irregular cortical thickening with a serpentine pattern. CT provides a more detailed view of the sclerosis, and MRI usually shows low signal intensity across all sequences due to the dense cortical sclerosis (6-8).

CAFFEY SYNDROME
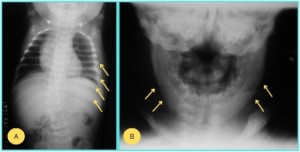
This is a rare disorder in infants, that is characterized by periosteal reaction and cortical thickening, particularly in the long bones, with swelling of soft tissues. Radiographs show periosteal new bone formation along the shafts of long bones, with cortical thickening and the characteristic "onion-skin" appearance. MRI reveals soft tissue swelling with abnormal signal intensities corresponding to the periosteal reactions. Though self-limiting, it can cause significant skeletal deformities in some cases (9, 10).
MAFFUCCI SYNDROME
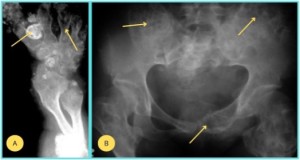
Maffucci syndrome is characterizaed by multiple enchondromas and soft tissue hemangiomas. On radiographs, the enchondromas appear as well-defined, radiolucent lesions with calcified ring-like patterns. MRI is helpful for detecting hemangiomas, which appear as well-defined, hyperintense lesions on T2-WI. This syndrome also has a higher risk of malignant transformation of enchondromas, making imaging surveillance critical (4).
OLLIER DISEASE
Ollier disease is similar to Maffucci syndrome but lacks soft tissue hemangiomas. The hallmark on radiographs is multiple well-defined enchondromas, most commonly in the metaphyses of long bones. CT and MRI may reveal lobulated masses with calcified areas. MRI is especially useful for monitoring changes in bone marrow and detecting malignant transformation, which can occur in some cases (3, 4).

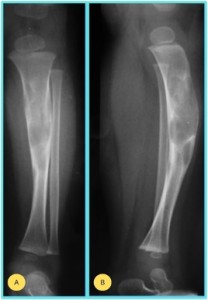
ENGELMANN-CAMURATI SYNDROME (ECS)
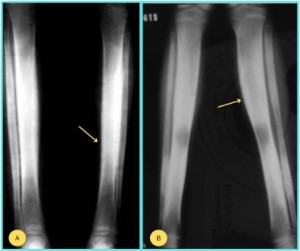
ECS, known as progressive diaphyseal dysplasia, is an uncommon disease. The diagnosis is based on the clinical symptoms and laboratory findings, but is confirmed by the radiological images. The characteristic radiological manifestations are fusiform cortical thickening of the long bones, bilateral and symmetric. CT and MRI help assess bone involvement, with MRI showing low signal intensity due to sclerosis and can also evaluate associated muscle atrophy (15).
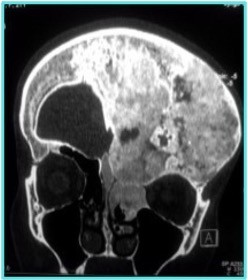
PAGET’S DISEASE
Paget disease is a chronic bone disorder characterized by excessive bone remodeling, usually affecting the pelvis, spine and long bones. Radiographs initially show a "coarsened" trabecular pattern, with cortical thickening and enlargement of affected bones, and a mixed lytic and sclerotic pattern. As the disease progresses, bones may become more brittle and deformed, with a characteristic "cotton-wool" appearance in the skull. CT and MRI provide better visualization of trabecular changes and cortical thickening, with MRI showing variable signal intensity depending on the phase of the disease (13, 14).